Tackling the health workforce is number one priority, says new Minister of Health Ayesha Verrall, as she expressed gratitude to nurses working in cyclone-affected zones.
“Their care means so much to their community right now and the assurance they’ve been able to provide, keeping the hospitals and community services open — I think that was really reassuring,” Verrall told Kaitiaki Nursing New Zealand.

“I just want to acknowledge, I know many of them are dealing with tough circumstances for themselves or their family, while providing that care.”
Verrall said addressing health workforce issues was top of her three priorities — followed by winter pressures, “by which I mean acute demand”, and hospital waiting lists.
“So that’s why workforce has to be the top priority . . . because it unlocks and makes possible all the other things we want to do. That’s not rocket science, is it?”
‘That puts us, for new nurses and experienced registered nurses, on par with Australia.’
Verrall said she saw first-hand the pressures faced by nurses when she visited Wellington, Lower Hutt and Rotorua EDs this month, shortly after her appointment. While she also had first-hand experience as a doctor, “it is clear they [pressures] are worse now than they were pre-COVID.”

Addressing staffing pressures in hospital operating theatres would also help get waiting lists down, while well-staffed aged residential care (ARC) facilities would allow patients to be discharged into care, she said.
“. . . we want young people to think ‘I want to be a nurse’.”
NZNO has estimated New Zealand is about 4000 nurses short, with many leaving for better pay and conditions in Australia.
In the long term, Verrall said she wanted the new health system to focus on “prevention, keeping us well in our communities and equitable outcomes.
“We have challenges but we also have the greatest opportunity in a generation to transform health care for the better.”
Relationship with nurses ‘prioritised’
Verrall said she would prioritise a “honest” and “open” relationship with nurses and NZNO, having met NZNO president Anne Daniels and chief executive Paul Goulter and talked to nurses in several ED visits immediately following her appointment.
“It’s important. We have many big issues to work through – the health system, and between Government and clinician groups, we just have to have open dialogue about it, and honesty.”
Former Health Minister Andrew Little incensed nurses last year when he refused to acknowledge the health system was in crisis, sparking an angry response from more than 2700 NZNO members.
‘It will take time to bring through new generations of nurses but the work to make the workplace a good place for Māori nurses to thrive has to start now.’
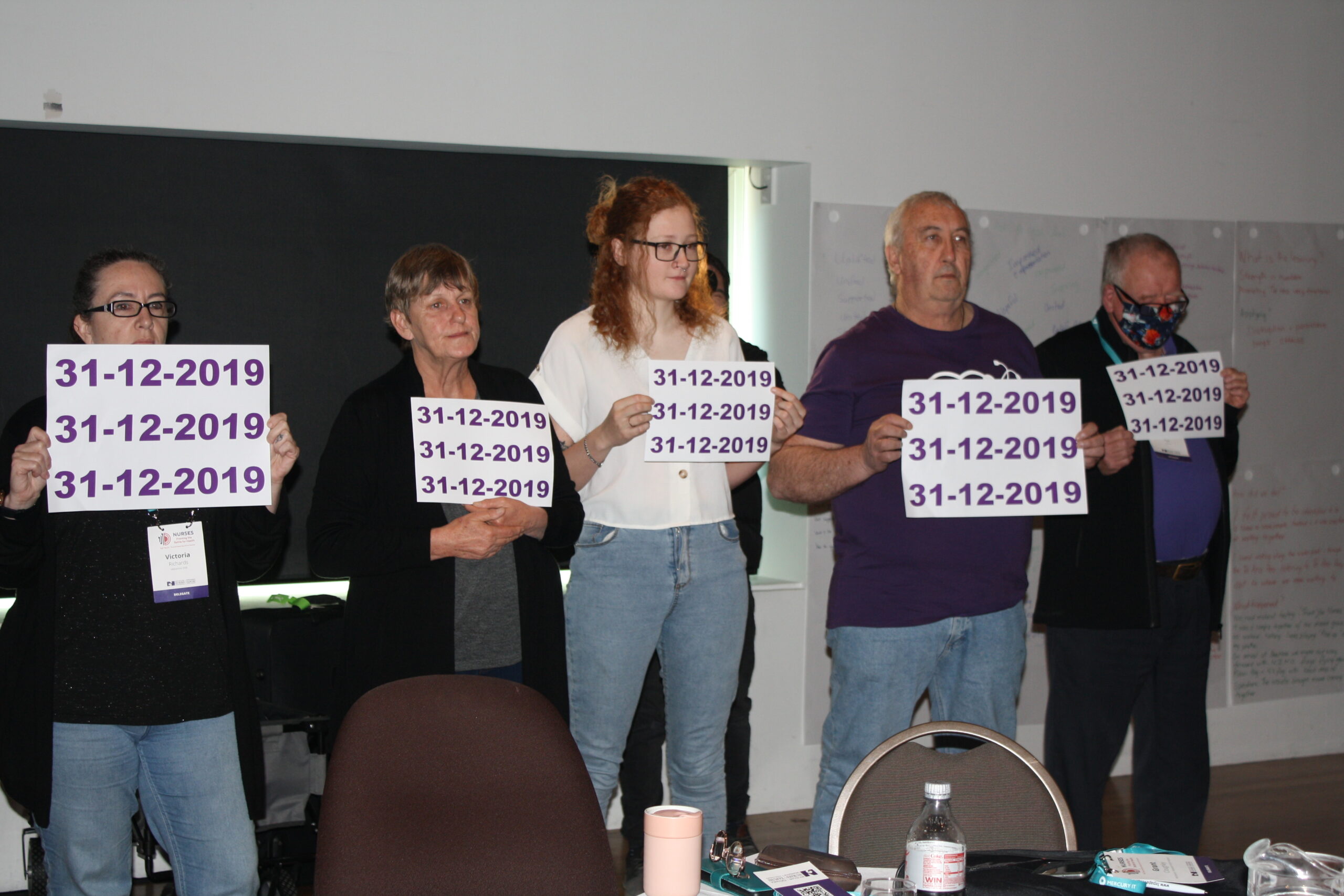
Further tensions arose with NZNO over both pay equity rates for Te Whatu Ora members, and whether the deal should be back-paid to December 2019. Court action over both pay equity rates and back pay is ongoing, despite Te Whatu Ora’s move to make an interim pay rise to its NZNO members late last year.
NZ nurses’ pay now ‘on par’ with Australia
Verrall said better pay was a key way to attract more nurses — and nurses’ salaries had been raised 25 per cent in the past six years under a Labour-Greens-led Government.
“That puts us, for new nurses and experienced registered nurses on par with Australia.”
The interim pay equity payments going out over the next couple of weeks would make further “substantial” progress, she said.
‘Nurses are irreplaceable in our health system and they will always do those things only nurses can do.’
“I think that is massive change in terms of the actual money and the relativity with Australia and demonstrates a true commitment to improving the issues.”
Verrall said it was important for people to be aware that trans-Tasman nursing salaries were now competitive. “On all sides of this we want young people to think ‘I want to be a nurse’.”
Verrall would not comment on the NZNO pay-equity rate dispute as it was before the Employment Court. However, she said she was “very happy” with Labour’s 2020 amendment to pay equity laws which now allow unions or individuals to raise gender-based claims directly with employers “. . .because we believe female-dominated workforces should have an avenue for addressing historical gender-based discrimination”.
Pay parity
Pay parity for all nurses, no matter where they worked, was “a priority” but “complex, because we don’t employ those nurses in those sectors directly”.
However, “I have heard NZNO on [pay parity],” she said.
In November, Andrew Little announced a $200 million annual sum to bring nurses and other health workers working for aged care, Māori/iwi and Pacific providers and hospices into line with their Te Whatu Ora peers this year. Mental health and addiction, organisations caring for the disabled and other residential care workers would follow — however primary health and practice nurses were excluded due to lack of evidence over a pay gap, he said.
The role of unregulated staff ?
A safe workplace was also crucial, Verrall said. Unregulated health-care workers had “risen to the call to help in health during COVID”, and she believed they could play a role in safely staffing hospitals — “for example, caring for people waiting in EDs, de-escalating some of the stress there that sometimes leads to our staff experiencing unacceptable abuse”.
Asked for assurances that nurses’ roles would not be usurped by unregulated workers, Verrall said nurses were “irreplaceable”.
“Nurses are irreplaceable in our health system and they will always do those things only nurses can do. I also hear from nurses that they are phenomenally busy, often with tasks that don’t draw on those very special skills that they have and that’s where other parts of the workforce can support them.”
Māori nursing workforce
More work was needed to make the health system a “good place for Māori nurses”, Verrall said. “It will take time to bring through new generations of nurses but the work to make the workplace a good place for Māori nurses to thrive has to start now,” she said.
‘We have challenges but we also have the greatest opportunity in a generation to transform health care for the better.’
“We’re not starting from zero – I trained clinicians in my job and I know there are already great initiatives around the country and we need to keep scaling them up and support the people who have been teaching that kaupapa for a long time already.”
The Māori Health Authority, Te Aka Whai Ora, was a “crucial” part of reforms in giving a voice to Māori in all decision-making, she said, pledging it would be safe under Labour despite apparent public fears about co-governance.
“Under a Labour Government, the Māori Health Authority will continue to grow and thrive so we get the health outcomes that we need for Maori and reverse the terrible inequities that we see.”
Hope for the future?
Verrall said she wanted to acknowledge the challenges faced by nurses — but also offer hope.
“The point is, when I visited Wellington Hospital, I remember working in that department as a medical registrar. I could see it looked really tough on the staff because of how busy [it was] and the patients waiting in corridors.
“As minister, I think it’s my job to be honest about that and acknowledge that it’s the truth, right? And then to point to the pathway of how we get out of this situation to a more sustainable situation.”

That was how she was trained, as a health professional, she said. “Be honest, but give hope about what you can do for people – it’s just the same.”
Verrall said she valued the voice of nurses, and understood the challenges of a hierarchical health system.
“As a specialist in tuberculosis, I realised that the trick to safe care for my patients was working in an even playing field with the nurses who were looking after the patients and the community. If you practise in a hierarchical way, you don’t hear the information that’s going to save someone’s life. So I think it’s very important to equal the playing field in terms of that voice.”
An expert on vaccines, tuberculosis and COVID-19, Verrall trained at Otago Medical School and worked as a junior doctor at Wellington, before training as an infectious diseases specialist in Singapore and researching tuberculosis in Indonesia.




