November 18-24 is World Antimicrobial Resistance Awareness Week (WAAW)
 World AMR Awareness Week aims to improve awareness and understanding of antimicrobial resistance (AMR). The New Zealand Antimicrobial Stewardship and Infection Pharmacist Expert Group (NAMSIPEG) has provided the following information to support this initiative.
World AMR Awareness Week aims to improve awareness and understanding of antimicrobial resistance (AMR). The New Zealand Antimicrobial Stewardship and Infection Pharmacist Expert Group (NAMSIPEG) has provided the following information to support this initiative.
About AMR
AMR is one of the top 10 global public health threats, causing over 1.3 million deaths each year. The biggest driver of AMR is use of antimicrobials, including overuse and misuse. AMR compromises routine and complex medical care, such as surgery and cancer treatment, where antimicrobials are needed to manage infection.
Learn more about AMR from the Ministry of Health Manatū Hauora , the World Heath Organization, the Australian Government and the European Centre for Disease Prevention and Control.
About WAAW 2023

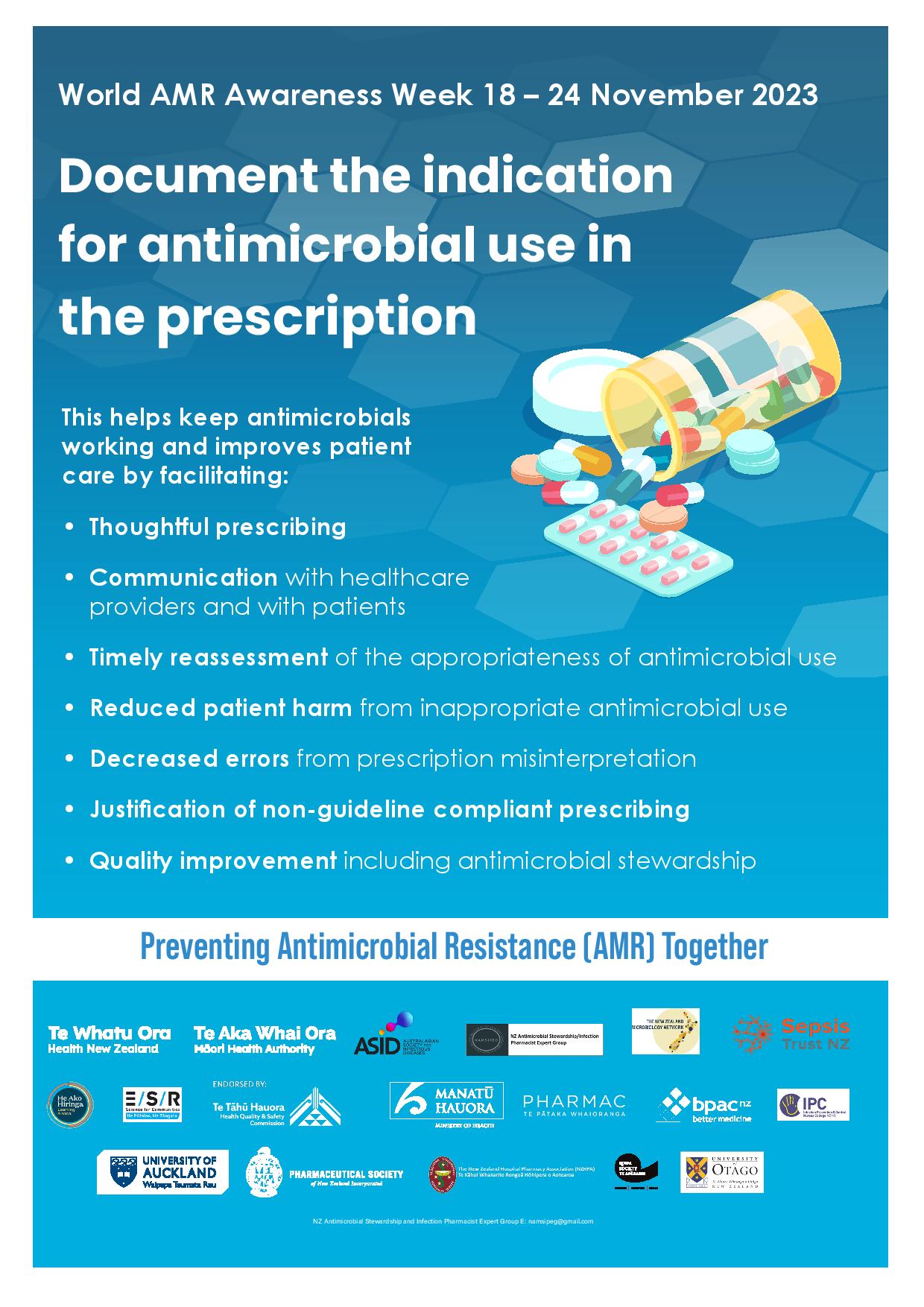
This year’s global theme is Preventing AMR together and our national theme is Indications in antimicrobial prescriptions. This means being specific about what the prescription is for, for example, write “cystitis” or “pyelonephritis” rather than “UTI” or “infection”.
Eighteen organisations have joined together in Aotearoa this year to promote documenting the rationale for antimicrobial use in the prescription. This action can help improve patient care and conserve antimicrobial effectiveness (see poster below).
A range of free resources (including posters, screen savers and this information as a printable bulletin) are available on the New Zealand Pharmaceutical Society website.

What can health professionals do to help slow AMR?
Use antimicrobials wisely by:
- only using them if the benefits likely outweigh the harms
- following relevant local guidelines and having a low threshold for seeking advice
- thinking the “4Rs” – right agent, right route, right dose and right duration
- challenging the veracity of penicillin allergies – see 2021 WAAW resources
- documenting the indication and course duration (ie, review or stop date) in the prescription.
Prevent infections and spread of resistant microbes by:
- washing hands regularly
- following relevant infection control guidelines
- ensuring safe food handling
- keeping vaccinations up to date
- encouraging safer sex practices
- avoiding unnecessary use of invasive devices such as IV lines, and removing them promptly when no longer required.
National antimicrobial guidelines 2024
Aotearoa has much duplication in antimicrobial guideline development at district, regional and national levels. This creates inconsistencies and is inefficient.
A team of clinicians is now working collaboratively across the motu to harmonise the existing guidelines into a national standard for antimicrobial prescribing. The guidelines will be freely available in both mobile and desktop versions and will be launched in November 2024.
Getting involved
The national antimicrobial guideline development is part of a suite of projects aimed at promoting effective, safe and equitable antimicrobial use. An introductory letter has been widely distributed. If you are keen to contribute, or are interested in hearing about progress, contact [email protected]
He Ako Hiringa tools to help slow AMR
EPiC dashboard
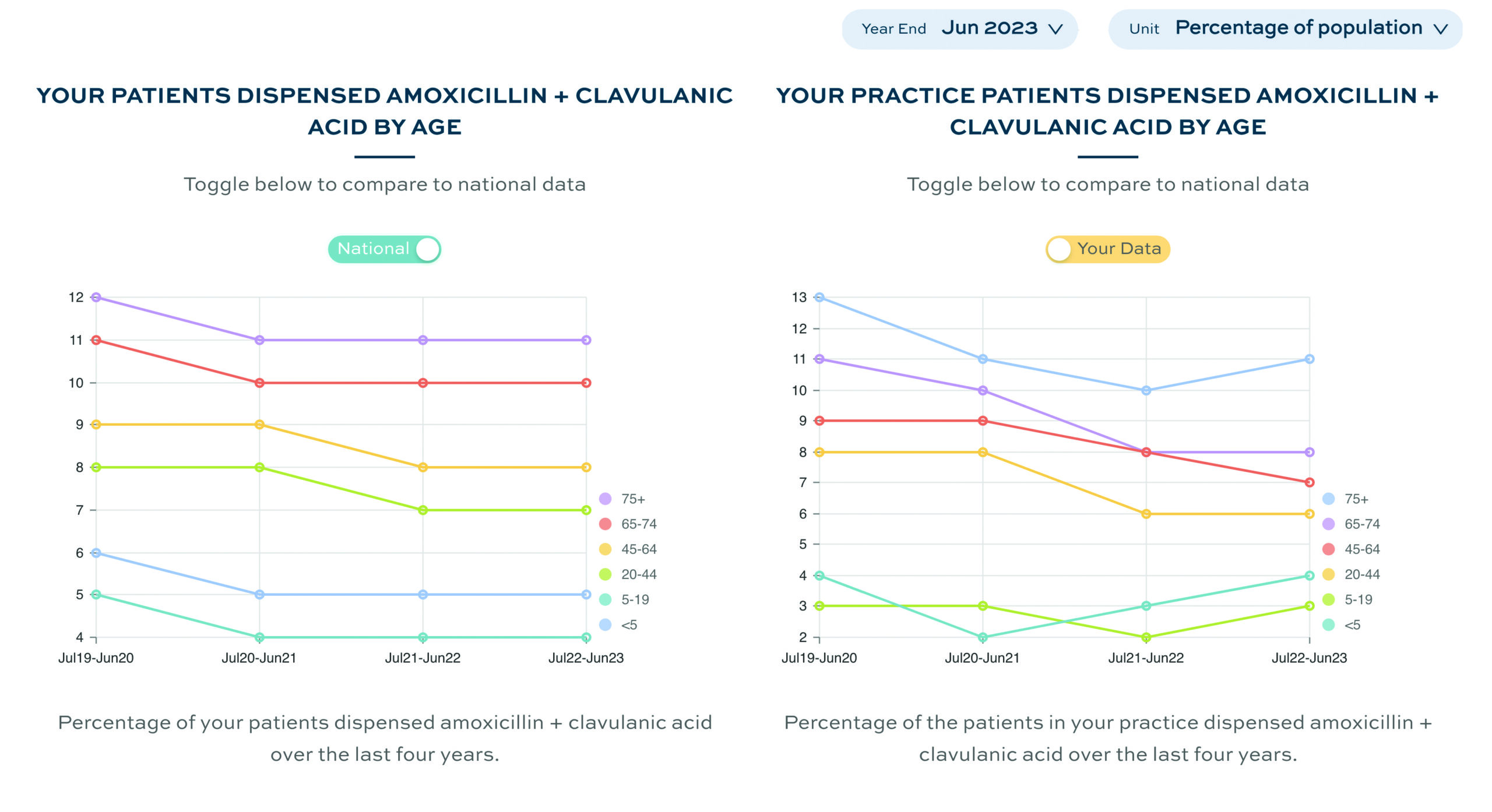
EPiC is a data analytics tool that enables clinicians to compare their own prescribing with prescribing for all patients in their practice and with patients nationally, using age, gender, ethnicity and socioeconomic deprivation quintile filters.
Community dispensing of antibacterials accounts for around 95 per cent of human antibacterial consumption in Aotearoa1 so small changes to practices in primary care can have significant effects on addressing antimicrobial resistance in the community.
The EPiC antibiotics dashboard helps clinicians to review their prescribing of antibiotics and consider areas where they might implement change. Data are included for urinary tract infection, seasonal variation, use of amoxicillin + clavulanic acid and use of topical antibiotics.
The CQI Toolkit
The continuous quality improvement toolkit consists of an activity guide, a data collection form and an information sheet. The resources guide you through identifying an area for improvement, collecting baseline data from EPiC antibiotics, implementing a change, and collecting subsequent data to determine if the change has been beneficial.
The toolkit uses antibiotic prescribing throughout the example templates, making it an ideal aid for improving antimicrobial stewardship and reducing AMR. The toolkit is endorsed by the RNZCGP to help medical practices meet various requirements of the Foundation Standard and the Cornerstone CQI and Equity modules.
Acknowledgements
WAAW content was obtained, with permission, from the November 2023 Antimicrobial Stewardship bulletin 041, written by Te Whatu Ora Waitaha Canterbury Hospital Antimicrobial Stewardship Committee in conjunction with NAMSIPEG.
Reference
- Duffy, E., Ritchie, S., Metcalfe, S., van Bakel, B., & Thomas, M. G. (2018). Antibacterials dispensed in the community comprise 85%-95% of total human antibacterial consumption. Journal of Clinical Pharmacy and Therapeutics, 43(1), 59-64.
Further reading
- Antimicrobial Resistance Collaborators. (2022). Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet, 399(10325), 629-655.
- World Antimicrobial Awareness Week (WAAW) will now be World AMR Awareness Week
- Kotahitanga – Uniting Aotearoa against infectious disease and antimicrobial resistance