During the first four months of the COVID-19 pandemic in New Zealand, there were 167 cases among health-care and support workers – 11 per cent of the 1504 total.
According to a Ministry of Health (MoH) report, 96 health-care and support workers with COVID-19 were likely to have been infected in the workplace. This represents 6.4 per cent of total cases. 1 Nine of the workers were hospitalised, with two needing intensive care. All recovered and there were no deaths.
More health-care assistants (HCAs)/caregivers in aged residential care (ARC) were affected, compared with other health-care and support worker groups. The majority of cases were part of a cluster, with very few instances of transmission in community health-care settings.
The report defines “health-care and support workers” as HCAs and caregivers, nurses, community support workers, doctors, allied health professionals (such as occupational therapists), and administration staff who work in a health-care setting such as ARC or a hospital. It also includes staff such as kitchen staff or security personnel who work in a health-care setting.
The first case of COVID-19 in a health care or support worker was reported on March 17, 2020. Of the 167 health workers diagnosed with COVID-19, 73 (43.7 per cent) were HCAs, caregivers or support workers, 49 (29.3 per cent) nurses, 16 (9.6 per cent) allied health professionals, 11 (6.6 per cent) administration staff, nine (5.4 per cent) doctors and nine in other occupations such as cleaners, students or catering staff.
Of the 167 cases, 60 (35.9 per cent) were found to have been infected outside the workplace (primarily transmission within their household or imported from overseas). For 11 cases (6.6 per cent), the source was unidentified but thought unlikely to be the workplace.
Workplace infections
Of the 96 health-care and support workers (57.5 per cent) who were likely to have been infected in the workplace, 42 people (25.1 per cent) were likely to have been infected by a patient, resident or client, and 32 people (19.2 per cent) were found to have been infected by another health-care worker.
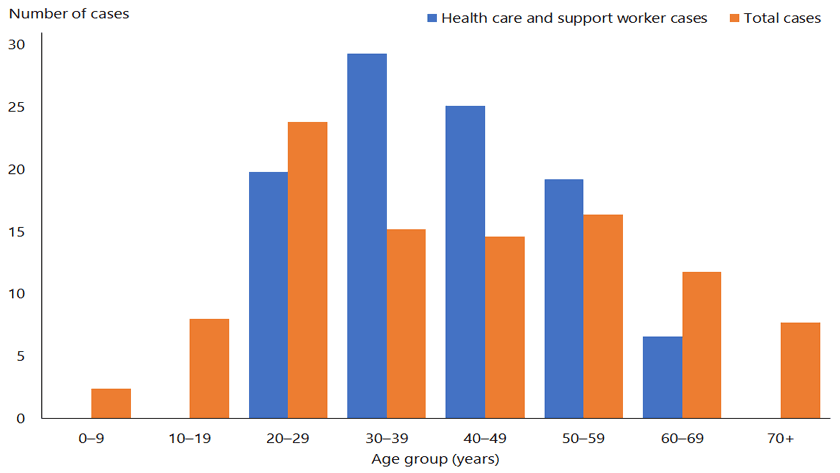
The age of infected health-care and support workers ranged from 20 to 69, with a mean age of 41. Around half the cases were European, 4.8 per cent Māori, 9.6 per cent Pacific peoples and 35.3 per cent Asian.
Of the cases, 132 (79 per cent) were linked to a cluster, compared with 46 per cent of all cases. While this includes clusters unrelated to health-care settings, three major clusters in ARC facilities accounted for nearly half (49 per cent) of all cases in health-care and support workers.
The district health board (DHB) areas with the largest number of cases were Canterbury (48), Waitematā (37), Waikato (21) and Auckland (18). The higher numbers of cases in these regions reflect clusters in these areas.
Of the 96 health-care and support workers who were infected in the work- place, 60 (62.5 per cent) worked in ARC, 26 (27 per cent) worked in a hospital and 10 (10.4 per cent) worked in the community.
The majority (76.7 per cent) of health- care workers in ARC were health-care assistants/caregivers and 20 per cent were nurses. In the hospital setting, the highest proportion of infections was among nursing staff (76.7 per cent) and HCAs/caregivers made up only 11.5 per cent of cases.
According to the report, the length of time spent with COVID-19 positive patients or residents is a factor in the risk of a worker being infected with COVID-19.
Seven of the 10 hospital-based nurses who were diagnosed with COVID-19 were caring for residents transferred from ARC, as was the one HCA in a hospital setting.
It is likely that 32 workers with COVID-19 were infected by another worker in the workplace. All but one of these cases were linked to a cluster and the majority were in the ARC setting.
Of the 167 health-care and support workers who had COVID-19, 50 were likely to have infected one or more people, either at home or in the workplace.
The report highlights the importance of protecting workers, particularly nurses and HCAs/caregivers working in ARC, as the country continues to respond to the virus.
NZNO’s acting associate professional services manager, Kate Weston, said it was disappointing but not surprising that most of the health-care workers diagnosed with COVID-19 worked in ARC.
“Aged residential care is often short staffed on a good day, and it was really, really stretched during COVID-19. Staff were telling us they didn’t have enough time to take a break, or access the correct personal protective equipment with the right visors or masks, and donning and doffing was a problem.”
Weston believes the whole country owes these workers a vote of thanks for the work they did, especially considering that the long-term effects of having the virus are still unknown.
The MoH is now implementing an action plan to address the recommendations made in the ARC cluster report.2 A cross-sector, multidisciplinary working group, with representatives from ARC, DHBs, public health units and unions, has been formed to develop a nationally-consistent approach to managing pandemics in ARC.
Weston would like to see a full review of the COVID-19 response.
‘A long and painful journey to recovery’
 Recovering from COVID-19 has been a long and painful physical and emotional journey for Waikato rest home clinical nurse leader Donna Glossop.
Recovering from COVID-19 has been a long and painful physical and emotional journey for Waikato rest home clinical nurse leader Donna Glossop.
Glossop was one of two registered nurses (RNs) at the Atawhai Assisi Home and Hospital in Hamilton to contract the virus in March. Three caregivers and three residents also contracted it, with 15 cases eventually linked to this first Waikato cluster.
Glossop is unsure how the virus first entered the 86-bed facility, though it may have been through the daughter of a resident visiting from Australia.
When a resident tested positive for the virus, 27 staff were sent home, tested and required to stand down for 14 days. At that point, Assisi lost 40 per cent of its staff, with a core group working extra hours and a number of volunteers stepping in to ensure residents were cared for safely. All residents had to stay in their rooms and eat meals alone for their own safety.
Glossop had six weeks off work. Although becoming “very sick”, she did not need to be hospitalised. “When I first went to my doctor, he thought I had some kind of virus and just needed to rest. But I kept on getting worse. My body ached all over, I had a sore throat, a terrible cough, was suffering extreme fatigue and shortness of breath. Even getting to the toilet became a struggle – I had to stop for a rest on the way.”
Glossop stayed locked in her room most of the time, even for her birthday. This was despite being a single mother and having a daughter with a baby living in the house. None of the family could leave the house, and they struggled to get their groceries and shopping delivered. “The kids were worried I would die.”
When the drains blocked, Glossop could not even find a plumber willing to come to the house due to fear of contracting the virus. One of her friends had to ring the COVID-19 helpline in Wellington and a contractor was eventually found.
“I felt like a leper. Having the virus had a huge impact on me and my family, and created a lot of anxiety for all of us. The pain in my hips was excruciating – I would say my symptoms were 100 times worse than ordinary ‘flu. I am very grateful for the daily phone calls I received from the public health nurse. She was so compassionate and understanding.”
Glossop was impressed how well Assisi managed to contain the virus. “A district health board response team provided guidance on infection prevention and control, outbreak management and the use of personal protective equipment [PPE]. The home also brought in eight caravans and campervans to house staff onsite, as some were unable to continue living in shared accommodation or with vulnerable family members. Every staff member put on and removed PPE when entering and exiting residents’ rooms. The cleaning routine was intense and continuous.
“A lot of people died during this lockdown period. We allowed family to visit their loved ones, but only in full PPE.”
Glossop is grateful the home is now back to running normally, with visitors welcomed and activities restarted. She is still suffering from fatigue and doesn’t feel as “bouncy” as she used to feel, but is confident she will gradually get her full strength back.
References
- Ministry of Health. (2020). COVID-19 in Health Care and Support Workers in Aotearoa New Zealand.
- Ministry of Health. (2020). Action Plan for the Recommendations of the Independent Review of COVID-19 Clusters in Aged Residential Care Facilities.