
Older rainbow people have often lived much of their lives in “terror” and hiding, TapIn diversity consultant Julie Watson told aged care nurses and caregivers recently.
‘ Sadly . . . we are seeing a massive turn back to conservative values’.
More than 60 people attended the NZNO college of gerontology nurses‘ conference ‘Onwards and Upwards’ in Wellington recently.
Until recently, Watson said she had been “delighted” at Aotearoa’s social progress on gender diversity. “But sadly it’s no longer that way — we are seeing a massive turn back to conservative values.”
With rising anti-trans movements overseas “flowing back” here via social media and through the profile of anti-trans activists such as Posey Parker, New Zealanders still needed to be “incredibly vigilante” to discrimination. This was especially the case in aged care where many had been treated their whole lives as if being gay was a mental health disorder.
“We know that two lesbians who lived together their whole adult life, took two units . . . because they came to the [retirement] village as ‘companions’, as ‘friends’ – no one was to know the true nature of their relationship.”
If you’re trans-gender or inter-sex, with a “non-standard” body — “a body that might shock people when they come to do personal care” — it can be “really tricky” in institutions set up for binary genders.
‘Walking past that behaviour means you’re kind of aligning yourself with the joke teller.’
Organisations may need gender-neutral bathrooms, paperwork such as admission forms that capture this type of information — “that’s something that really needs to be thought about” — along with using neutral pronouns such as “they”.
“We know a lot of people carry a lot of fear of coming out as an older person . . . So spending time with someone who you suspect is experiencing some kind of distress you can’t put your finger on, maybe it’s that queerness that they don’t feel able to express.”
Being a ‘true ally’
Watson said being a true ally to the rainbow community means “you don’t walk past bad behaviour.

“If you see someone telling a homophobic joke, telling a transphobic story, treating somebody without the dignity they deserve because of them being rainbow — walking past that behaviour means you’re kind of aligning youself with the joke teller.”
‘This is a really loving thing that people live in this world, and just adjust the headspace’.
Wearing a visible sign of support such as a rainbow button, ribbon or bracelet — “anything to show the people you’re working with you’re an ally” — would also make a huge difference to people.
“All of those things might seem small, might seem token, might seem insignificant – but for the people who need to see them, they’re like a neon sign, they’re very, very visible.”
Continually educating oneself on the rainbow world was also essential for caregivers, Watson said.
‘Giant journey’ for some staff
High numbers of aged residential care (ARC) staff came from overseas, often countries where anything rainbow was “extremely illegal” and harshly punished, Watson said. Working in a country where the minister of finance is a gay man may be “hard to reconcile” initially, Watson said.

“There always needs to be some tolerance and acceptance that people might take a while to have that soak into their soul. In this country it’s different and this is not illegal — and this is a really loving thing and just adjust their headspace.”
Being queer, or rainbow, includes:
- sexual orientation — about relationships and who you love.
- gender — about identity. Who am I? How do I express myself to others?
- sex characteristics — about the physical characteristics people are born with, their hormones and chromosomes.
Person-centred care

University of Sydney professor of nursing Brendan McCormack spoke about the importance of making aged care facilities flourishing and “passionate” places for staff and residents — “that we want to turn up to, day after day”.
‘I still have potential to flourish as a human being and that should never, never be taken away from me.’
“Our goal, as registered nurses [RNs], is to help older people in our care to flourish. That is our only job.”
Focusing on technical tasks such as medications, bowel motions, diet, “I find offensive — that is not our main job,” McCormack said. “Our job is to put the framework around those activities that enables them to be the best that they can be, that helps that person flourish.”
Older people, like everyone, wanted “to actually live”, not just exist.
‘It’s something we’re going to have to rethink as aged care nurses, as [at home] will be where we do our gerontology.’
“Flourishing is the highest good, it’s the thing we all strive for in our lives – and there is no point in our lives when we shouldn’t still be flourishing, no matter how much dementia I have, how disabled I am – I still have potential to flourish as a human being and that should never, never be taken away from me.”

There were many challenges to implementing person-centred care, such as nursing education, regulatory frameworks, workforce shortages and weak nursing leadership.
But nurses could still “rethink their role”, focusing less on tasks, instead on helping people to:
- maintain their health by managing symptoms and risks well.
- manage distress and pain including mental health.
- maximise potential – “how do we help people to cope with things in their lives, to have ambition, hope dreams, desires — to continue to contribute to life”.
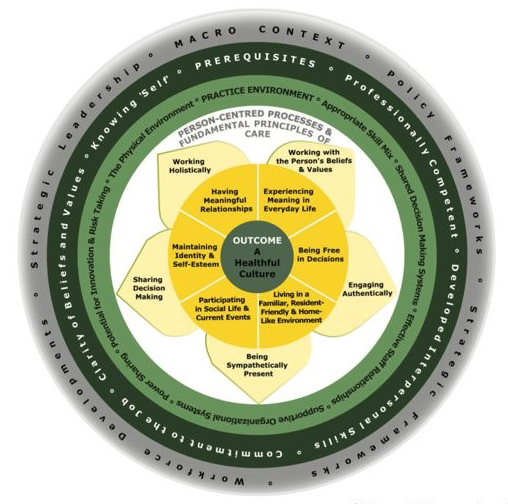
“If we can do that, I think we can transform the role of the RN in aged care.”
Growth in home-based aged care
There was also a move away from residential aged care towards home-based aged care, particularly in parts of Asia, he said.
“It’s something we’re going to have to rethink as aged care nurses, as that will be where we do our gerontology . . . How do we do that in a way that is respectful? That is not just a sticking plaster or a 15-minute visit and the like – but actually really genuinely offers care and support for people in their homes?”
In Australia, where he worked, the recent Royal Commission of Inquiry into aged care quality and safety had raised “profound” issues and had led to huge investments in aged care and a 15 per cent increase in aged care nurses and other workers’ pay.
Further information about person-centred care can be found at: www.pcp-icop.org.
Waikato aged care nurse practitioner/mātanga tapuhi Bridget Richards said it was exciting to be gathering face-to-face after four years of COVID-forced isolation, but warned aged care was close to “rock bottom” in terms of short-staffing.

Canterbury’s Kōwhai programme coordinator Fiona Graham also talked about the benefit of providing skilled companionship to older people in hospital.
In the Canterbury region, there were now 53 trained Kōwhai companions providing one-to- one person-centred “safe, compassionate” care to vulnerable people — those with dementia, depression, hearing or vision impairment — which could reduce cases of dementia by up to 30 per cent.
She shared some clips of volunteers who said the older patients had also taught them things, like “not to sweat the small stuff”.
“They just tell me all their stories, I just take them down for coffees – and at the end of the day I can tell it’s made a big impact and put a big smile on their face. I can go home feeling really good knowing I made a difference to someone’s day.”
At its annual general meeting, the college also agreed to open its membership to include nursing students.





