We write this on behalf of, and in close collaboration with, an informal taskforce for nursing; a sector-wide group of nurse leaders with shared concern for the current political environment and the consequences for nursing services.
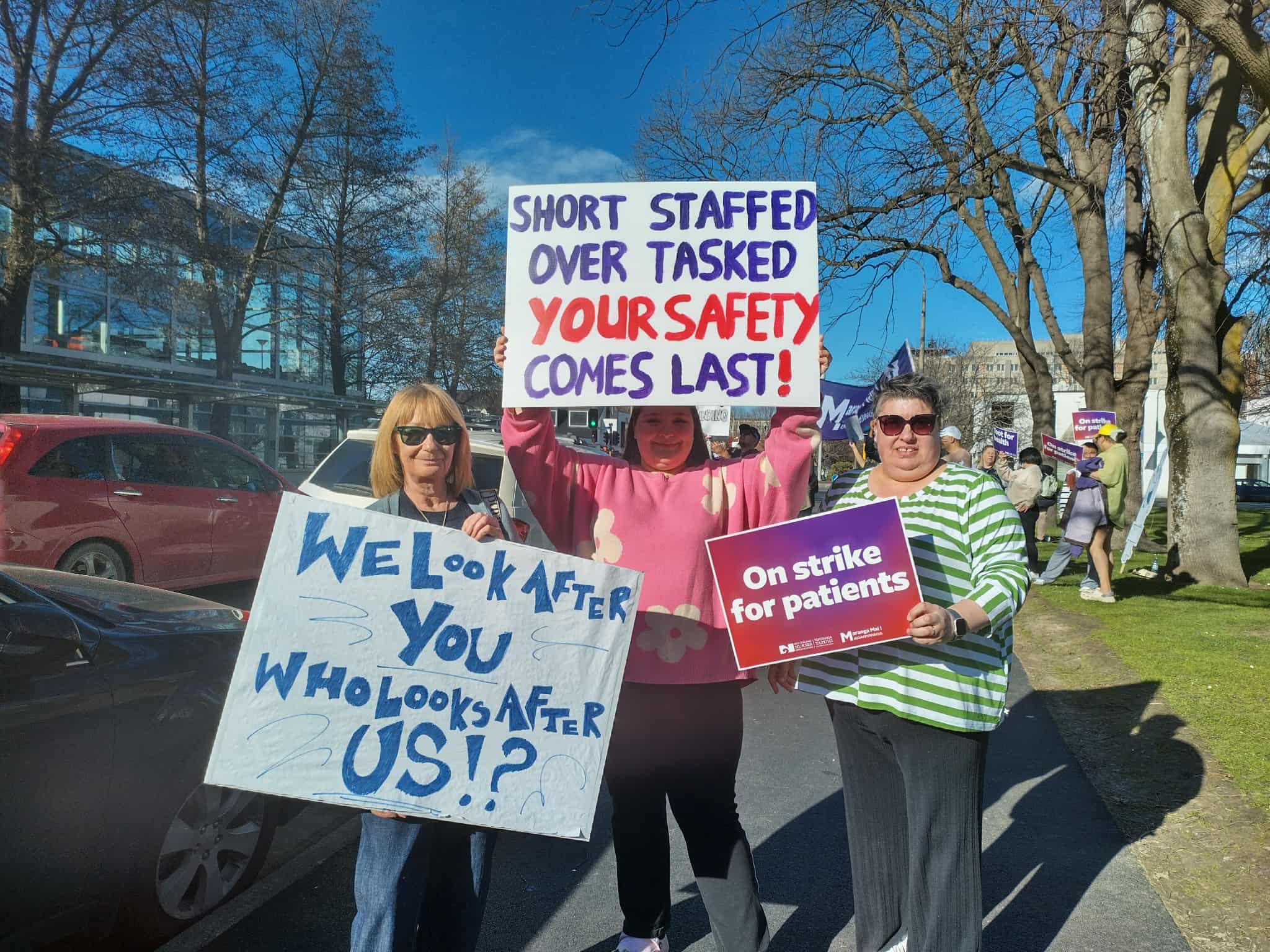
Nurse leaders with direct accountability for patient safety are being silenced by organisational policy. The Minister of Health, Simeon Brown, expressed disappointment that nurses intending to strike were forgetting to put patients first. Given that the principal concern of striking nurses is safe staffing, his comment is paradoxically inattentive. Safety is a critical issue in health service provision; low staffing levels or insufficiently trained nurses increase the risks of mortality and morbidity.
One in every eight patients in New Zealand hospitals suffers an adverse event during their stay. There is a strong association between nurse staff level, skill mix, and patient safety in hospitals. Data collected across 12 million patient discharges in New Zealand showed that as registered nurse numbers drop, adverse outcomes rise steeply.

International work has shown that when nurses care for too many patients, readmissions increase and 30-day mortality after surgery rises. ACC payments for treatment-related injuries, including infections, pressure injuries, and drug errors, more than tripled from 2015-2016 to 2023-2024. Most of these indicators are related to staffing levels. As nurses witness these failures of care, they experience significant distress and many leave, adding turnover costs to the cost of risks associated with poor staffing levels.
New Zealand is led by a coalition Government driven to engage in a bleaching of the social and health service environment.
We are engaged in the practice of democracy by seeking to contribute to society and its values and priorities – drawing attention forcibly to the safety of people accessing and receiving healthcare. As nurses we engage with people ill or injured in the context of their lives, culture, and economic realities. Supporting people to maintain wellbeing, understand their conditions and self-manage their symptoms is vital to good outcomes.
For people to participate in their health they need to feel safe. Those who do not risk poorer health. Nurses understand that safety is a concept that includes clinically and culturally safe care, recognising the intersections between power, health disparity, ethnicity, and socio-economic determinants in the giving and receiving of care.
New Zealand is led by a coalition Government driven to engage in a bleaching of the social and health service environment. There is a strong attempt to frame any discourse that draws attention to differences of any kind as racist. In such a context, nursing’s long-standing commitment to the provision of culturally-safe care is under attack through the proposed “Modernising Health Workforce Regulation” consultation and the onslaught of ill-formed critique from ACT MPs. The proposals seek to remove the autonomy of the individual professions in regulating themselves. A key target is cultural safety.

Delivering culturally safe care for all is also threatened by proposed revisions to the Pae Ora (Healthy Futures) Act 2022. Along with the petty revision of the title to Healthy Futures (Pae Ora), it will remove Te Tiriti o Waitangi commitments and protections, and Māori health targets. The Bill also mandates the removal of requirements for Public Health Advisory Committees to have knowledge of and experience and expertise in population health, health equity, Te Tiriti o Waitangi, epidemiology, health surveillance, health promotion, health protection, or preventative health. Other amendments remove ethnicity-based eligibility criteria for funded services.
Safe, cost-effective care in all health service settings depends on safe staffing levels. Due to an unacknowledged workforce hiring freeze, workforce burnout, the effects of underfunding, the destruction of pay equity pathways, and differential nursing pay rates across sectors, staffing is rarely adequate. Poor staffing in itself creates high levels of attrition through moral distress and exhaustion. The recent failures to employ more than half of new nurse graduates will increase the flow of nurses out of the country. Many remaining new graduates will also only be employed on less attractive part-time contracts.
Along with the petty revision of the title to Healthy Futures (Pae Ora), it will remove Te Tiriti o Waitangi commitments and protections, and Māori health targets.
All of this is deeply ironic in a situation where the Government is myopically focused on cost-saving. Poor staffing and culturally unsafe care directly influence costly failures (short- and long-term) not to mention the associated distress and suffering. Overt and covert plans to privatise the health service will further spread a thin workforce over multiple environments and again disadvantage those who most need care, engendering long-term escalation of costs in health, education and justice.

Lester Levy, chair of Health NZ/Te Whatu Ora, noted in a recent editorial in the New Zealand Medical Journal that “Every operational choice – from workforce planning to service redesign – must be viewed through the lens of patient benefit”. We concur and would extend benefit to also include community benefit. But we are left wondering if safe staffing and equity of outcomes will be core features of future planning.
— Jenny Carryer is a professor of nursing at Massey University, Andrew Jull is a professor in the school of nursing at the University of Auckland; Professor Nicolette Sheridan is director of the centre for nursing and health research at Massey University.
This column was first published in The Post and reproduced with permission.





