Registered nurses (RNs) and student nurses have the most contact with patients. Therefore, it is essential that both these groups use effective hand hygiene techniques to prevent hospital-acquired infection in patients.1
RNs also need to be accountable for ensuring hand hygiene is performed adequately by other health professionals.2 However, during recent clinical placements we all witnessed incidents of inadequate hand hygiene, including an RN drying her wet hands on the back of her uniform. This is alarming in a world experiencing a deadly pandemic.
New Zealand Government and health officials have emphasised the importance of hand washing to stop the transmission of COVID-19.3 This article discusses the pressures on nurses that undermine the gold standards of hand hygiene in the workplace. We explain the notion of the five moments of hand hygiene, and present reasons why hand hygiene can be a struggle for RNs. We give examples of exemplary hand hygiene compliance and make recommendations to ensure RNs provide a hygienic environment for patients.
Defining the gold standard of hand hygiene
The World Health Organization4 has devised a “five moments for hand hygiene” framework, which is considered the gold standard for optimal hand hygiene in health care.5 It specifies that care providers must wash their hands
- before touching a patient,
- before aseptic procedures,
- after body fluid exposure or risk,
- after touching a patient,
- and after touching a patient’s surroundings.4
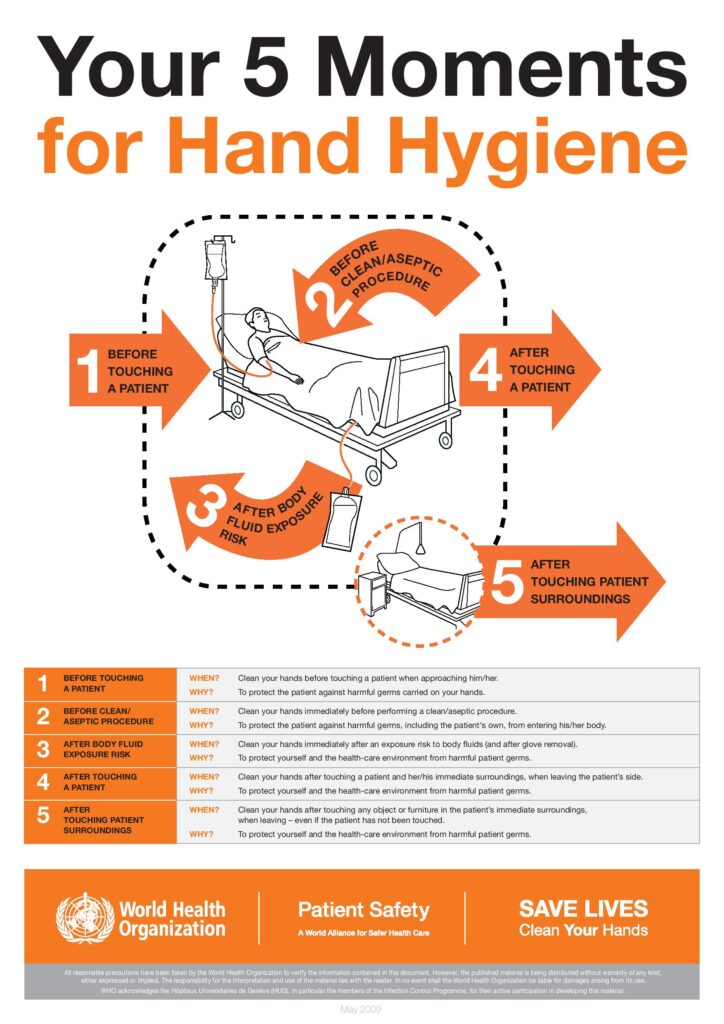
New Zealand health services use the WHO’s “five moments” approach so health-care workers can provide safe care for patients and minimise risk of and transmission of infection to patients and themselves.6 Principle 4 of the Nursing Council’s Code of Conduct for Nurses7 prompts RNs to employ health-care interventions to maintain consumers’ trust. This requires competent RNs to nurture hygienic environments.
The five moments of hand hygiene is a simple and effective strategy to break the chain of infection.
Many countries around the world use the five moments as their gold standard for hygiene compliance, but studies often find that awareness and observance of the five moments are low.8 A study in South Africa found that RNs had the most inadequate hand hygiene compliance of all health-care professionals, with a prevalence of 15.76 per cent.9 This finding shows the importance of RNs improving their hygiene skills as they are the health-care professional most in contact with patients. However there are barriers which can make this a challenge.
Contributors to poor hand hygiene

Deterioration of hand hygiene practices may reflect systemic issues in modern health care.10 RNs have heavy workloads, leaving little time for washing hands properly. Another contributor to poor hand hygiene may be that wards lack the necessary facilities.10 Problems can include empty or broken hand sanitisers. This makes maintaining hand hygiene harder, and fixing equipment adds to nurses’ already heavy workloads.
Moreover, patient-centred care requires nurses to place a higher priority on attending to patient needs than changing a sanitiser dispenser. Intergenerational factors could also potentially induce maladaptive hygiene practices. One study found a decline in performing hand hygiene among third-year nursing students, compared to first-year nursing students. This was attributed to the third-year nursing students seeing their preceptors washing their hands incorrectly.11
Positive measures we observed
The availability and effective placement of hand hygiene resources, including hand sanitisation stations and hand gels, is essential for the successful implementation of hygiene guidelines.12 On placement, we also saw aspects of hand hygiene that were working well. An example of this was the provision and consistent maintenance of hand hygiene equipment. Bottles of cleansing gel were placed at each patient’s bedside and at the entrance to every patient room. Also, several handwashing stations — consisting of a basin, hand soap, and paper towels – were placed throughout the ward. These measures contributed to the frequency at which RNs practised the five moments of hand hygiene.
On placement, we also saw aspects of hand hygiene that were working well. An example of this was the provision and consistent maintenance of hand hygiene equipment.
Another positive measure we observed involved tracking hand-hygiene compliance. One nursing student observed the charge nurse writing how well hand hygiene was being performed on the whiteboard in the nursing station. This served as a visual reminder for nurses to uphold hygiene standards and meet the criteria of the ward. The charge nurse held fortnightly meetings to discuss the observed data and hand hygiene compliance. This regular auditing appeared to be effective in maintaining adequate hand hygiene practices.
Recommendations
The latest NZ data
Hand hygiene compliance in New Zealand health facilities has remained high and improved during the COVID-19 pandemic, the Health Quality & Safety Commission (HQSC) says.16
The HQSC audits compliance with the WHO’s five moments for hand hygiene framework. Its most recent hand hygiene compliance report (covering July to October 2021) found 16 of the 20 district health boards (DHBs) were at or above the target 80 per cent compliance rate, as were 17 of 21 private surgical hospitals (PSHs).
The aggregate national compliance rate for DHBs was 87.5 per cent, compared to 86.2 per cent in the previous audit period. For PSHs, national compliance was 82.4 per cent.
The HQSC said the four DHBs who didn’t reach 80 per cent were not far away from it, rating 77.6 percent or above.
In DHBs, nurses and midwives had a compliance rate of 90 per cent, student nurses and midwives 87.7 per cent, and doctors 81.6 per cent. The HQSC said this audit period was the first time medical professionals had reached a compliance rate of 80 per cent or more.
The approach to achieving good hand hygiene is multifaceted: there are numerous ways RNs can work to bring about the best outcomes. As previously mentioned, the charge nurse resuming responsibility for the ward is a starting point. A systematic review carried out in 2019, showed that interventions based on leadership and social support promote long-term adherence to hand hygiene.13 Therefore, charge nurses should be active agents in their ward by tracking hand hygiene compliance to ensure that all RNs on the ward undertake their duty with due diligence.
A 2017 systematic review14 sought effective intervention to improve compliance among nurses. The most common ways hand hygiene compliance was improved were through education and workplace strategies. Education is the most fundamental, as every RN has been instructed to wash their hands during basic training. Student nurses are responsible for ensuring their hand hygiene is carried out correctly.15 Nursing students should take notice of poor hand hygiene habits and learn from their preceptors. If the student nurse is performing inadequate hand hygiene, the RN is responsible for observing and educating the student.14
Reminders around the workplace, such as posters and signs prompting nurses to wash their hands and showing the proper way of doing so, are credited as one of the main ways of improving hygiene.14 This strategy benefits not only nurses but everyone else on the ward. Since the posters will be displayed on the walls for all to see, patients and their friends and family can see that they must also play their part in maintaining hand hygiene.13 It is essential to share this hygiene knowledge with patients and visitors as not everyone knows how to do it.2 This strategy will thus sponsor a culture that promotes hand hygiene and popularises it among the wider community.
Role modelling plays a vital role in ensuring that hygiene practices are performed to a commendable standard. This means that RNs must remain disciplined when washing their hands so the students can witness the correct hygiene methodology. When the nursing student is completing duties for patients, it is then crucial for preceptors to supervise them and push them to maintain the five moments.11 The role of the student nurse is to seek help if they are not sure about the five moments, by attending lectures related to hand hygiene, searching online for guidance, and practising it during clinical placement.11
These recommendations will ensure that RNs establish accountability in the health-care setting and uphold high health and safety standards.
Conclusion
In today’s international circumstances, good hand hygiene is imperative. The five moments of hand hygiene is a simple and effective strategy to break the chain of infection. Adequate hand hygiene facilities are required, but it is also crucial to raise awareness about good technique. RNs, as health professionals, must practice strict hand hygiene and encourage nursing students to do the same. Through implementing strategies in and out of the workplace, RNs can do their part to ensure proper hand hygiene in the nursing profession.
Keenan D’Souza, Katarina Campbell, Amjad Alsiyabi, Sally Davis, Lucy Hou and Rebecca Zhao are third-year nursing students at the University of Auckland. Jackie Williams, RN, BN(hons), is a professional teaching fellow in the University of Auckland School of Nursing, and is the students’ academic supervisor.
-
- This article was reviewed by Jo Stodart, RN, MPH, an infection prevention and control charge nurse at Southern District Health Board and a member of the Infection Prevention & Control Nurses College NZNO.
References
- Sickbert‐Bennett, E. E., DiBiase, L. M., Willis, T. M. S., Wolak, E. S., Weber, D. J., & Rutala, W. A. (2016). Reduction of healthcare‐associated infections by exceeding high compliance with hand hygiene practices. Emerging Infectious Diseases, 22(9), 1628–1630. https://doi-org.ezproxy.auckland.ac.nz/10.3201/eid2209.151440
- Perkins, A. (2017). Hand hygiene. Nursing Made Incredibly Easy! 15(6), 1–7. https://doi.org/10.1097/01.nme.0000525554.52280.69
- Wilson, S. (2020). Pandemic leadership: Lessons from New Zealand’s approach to COVID-19. Leadership and the Coronavirus Crisis, 16(3), 279-293. https://doi.org/10.1177/1742715020929151
- World Health Organization. (2021). Save lives – Clean your hands.
- Gould, D. J., Drey, N. S., & Creedon, S. (2011). Routine hand hygiene audit by direct observation: Has nemesis arrived? Journal of Hospital Infection, 77(4), 290-293.
- Roberts, S., Freeman, J., & Jowitt, D. (2016). Hand hygiene New Zealand: The value of a national program in achieving and sustaining hand hygiene performance. In Open Forum Infectious Diseases (Vol. 3, No. suppl_1). Oxford University Press. https://doi.org/10.1093/ofid/ofw172.1074
- Nursing Council of New Zealand. (2012). Code of Conduct for Nurses.
- Woodard, J. A., Leekha, S., Jackson, S. S., & Thom, K. A. (2019). Beyond entry and exit: hand hygiene at the bedside. American Journal of Infection Control, 47(5), 487-491.
- Bale, T. L. A., Ramukumba, T. S., & Mudau, L. S. (2021). Evaluation of compliance to the World Health Organization’s five moments of hand hygiene: Cross-sectional observation of healthcare professionals. Southern African Journal of Infectious Diseases, 36(1), 255. https://doi.org/10.4102/sajid.v36i1.255
- Bezerra, T. B., Valim, M. D., Bortolini, J., Ribeiro, R. P., Marcon, S. R., & Batista Moura, M. E. (2020). Adherence to hand hygiene in critical sectors: Can we go on like this? Journal of Clinical Nursing, 23(13-14), 2691-2698.
- Magaldi, M. C., & Molloy, J. (2010). Using Student Nurses as Hand-Washing Ambassadors. Nurse Educator, 35(5), 183–185. https://doi.org/10.1097/nne.0b013e3181ed8189
- Hand Hygiene New Zealand. (2009). Guidelines on Hand Hygiene for New Zealand Hospitals. https://www.dcnz.org.nz/assets/Uploads/Consultations/2015/Infection-prevention-control-submissions/Att-2-CDHB.pdf
- Martos-Cabrera, M. B., Mota-Romero, E., Martos-García, R., Gómez-Urquiza, J. L., Suleiman-Martos, N., Albendín-García, L., & Cañadas-De la Fuente, G. A. (2019). Hand Hygiene Teaching Strategies among Nursing Staff: A Systematic Review. International Journal of Environmental Research and Public Health. 16(17), 3039. https://doi.org/10.3390/ijerph16173039
- Doronina, O., Jones, D., Martello, M., Biron, A., & Lavoie-Tremblay, M. (2017). A systematic review on the effectiveness of interventions to improve hand hygiene compliance of nurses in the hospital setting. Journal of Nursing Scholarship, 24(2), 143-152.
- Lillekroken, D. (2019). Teaching Basic Nursing Care: Nurse Preceptors’ Perceptions about Changing the Teaching Context from the Clinical Setting to a School Simulation Lab. International Journal of Nursing Education Scholarship, 16(1). http://dx.doi.org/10.1515/ijnes-2018-0033
- Health Quality & Safety Commission. (2021). National hand hygiene compliance report.




