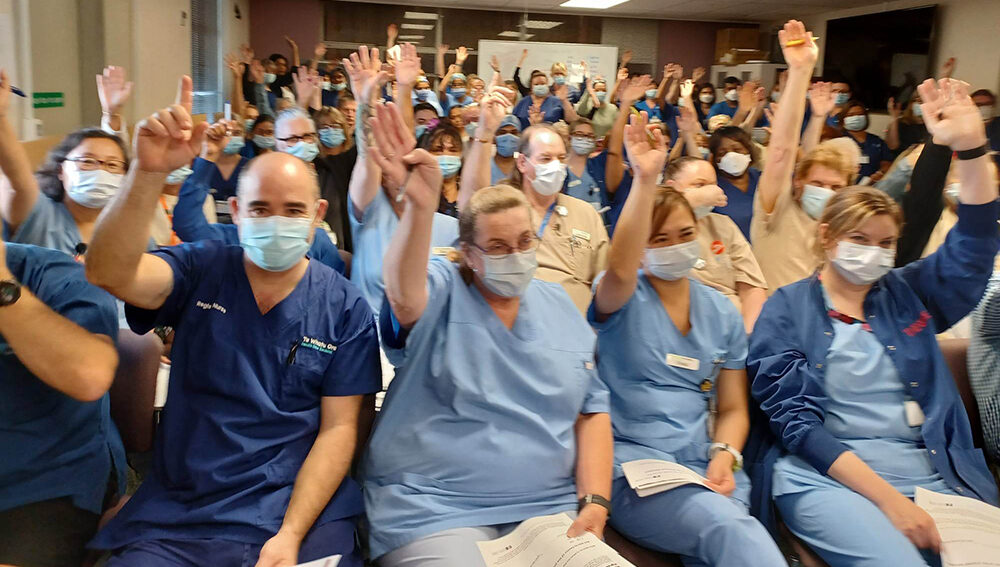
Thousands of members voted on whether they wanted the bargaining team to continue the fight for an acceptable deal — or not.
The bargaining team organised the stop-work meetings to discuss an offer, which they said fell well short of the claims.
Te Whatu Ora’s initial offer follows bargaining for a new multi-employer collective agreement (MECA) between NZNO members and Te Whatu Ora, which has been underway this year.
Results of this week’s ballot will be available next Tuesday, June 6.
The offer included a $4000 increase to all base salaries from April 1, 2023, and a further increase of either $2000 or three per cent (whichever is the higher) to all base rates on April 1, 2024.
‘It’s disrespectful to nurses, midwives, health care assistants — the whole profession.’
Back pay is not offered between the expiry of the collective agreement on October 31, 2022, and the increase in rates from April 1, 2023. Instead, Te Whatu Ora proposed a lump-sum payment of $500 (pro rata) to recognise the delay.
A claim for minimum staffing levels based on staff-patient ratios for all areas – including where care capacity demand management (CCDM) was not in place or fully implemented – was not part of the Te Whatu Ora offer.
‘I think nurses are absolutely sick and tired of being treated with total disrespect, with being left out in the cold.’
Likewise a claim for a tikanga allowance — in recognition of instances where clinical staff use their te ao Māori knowledge and tikanga to support Te Whatu Ora’s cultural obligations — was not part of the offer.
Tōpūtanga Tapuhi Kaitiaki o Aotearoa — NZNO president Anne Daniels said having large, collective, in-person meetings off-site provided an important opportunity for members, and was a visible sign of strength.

The previous collective agreement negotiations in 2020 took place against the backdrop of a global pandemic. Stop-work meetings were held at various on-site locations, at multiple times, but were understandably poorly attended, Daniels said.
Daniels attended a stop-work meeting at The Edgar Centre in Dunedin on Thursday and said the venue was “packed out”.
‘We’re asking you to tie a knot to hold onto with NZNO so we can go back to bargaining and try and improve this offer.’
“The feeling was very, very subdued and people are very angry towards Te Whatu Ora. The words ‘disrespected’ and ‘disgusted’ were used quite liberally,” she said.
In Christchurch on Thursday, over 600 members from Christchurch, Burwood, Hillmorton and Princess Margaret hospitals travelled by coaches and buses to the Riccarton Racecourse event centre. The 400-seat venue was packed, with many members standing for the 45-minute meeting.
Delegates and members of the Te Whatu Ora collective agreement bargaining team Al Dietschen and Debbie Handisides talked through the main aspects of the offer, and took questions before members voted on a resolution to accept the offer or return to bargaining.
‘Ridiculous’ offer
Christchurch Hospital plastics outpatients registered nurse (RN) and delegate Kirsty King said she thought the offer was “absolutely ridiculous”.
“It’s not even worth considering, yeah, no. It’s disrespectful to nurses, midwives, health care assistants (HCAs) — the whole profession. It just proves how little the Government thinks of our profession and what we do in health care.”
‘This korowai, an obligation to care for ourselves, our whānau and our communities.’
King said her biggest concern was safe staffing, and a claim for minimum staff-patient ratios.

King said her unit was “so short” of staff due to illness, as they were not able to use pool staff.
“It just means that the time isn’t spent [with the patients], that you would normally spend with them, they’ve just come in with a cancer diagnosis, but sometimes you can’t be there because you’re needed elsewhere, because you’re short.”
In Wellington, nurses, HCAs, midwives and kaiāwhina streamed out of Wellington, Hutt and Keneperu Hospitals at 2pm on Thursday and travelled by bus to their meeting in the Lower Hutt town hall.
More than 500 health workers filled the hall, some with their babies and toddlers. One nurse, Haley Johnson, had come from Otaki with her child to attend.
“I want to support everyone, I think turnout is the most important think – safe staffing is the main issue,” she told Kaitiaki.
Staffing ‘unsafe’

Concerns over unsafe staffing levels were echoed by many.
Wellington community health HCA Karen Don said staffing was the key issue for the region’s district nurses.
“Is it April Fools’?” she said of Te Whatu Ora’s lack of response over safer staffing and conditions proposed by NZNO.
Short-staffing meant community patients were often deferred for wound care, showering or incontinence support, Don said.

Even palliative care in the community was stretched to ensure enough staff were available to attend, she said.
Hutt Hospital nurse Naomi Waipouri said members wanted fair pay and safe staffing, now — and for Te Whatu Ora not to accept this was “negligence to not only their employees but also to the public”.
Of the turnout, Waipouri said: “It was like a blue and purple korowai that blanketed the Hutt Valley. This korowai, an obligation to care for ourselves, our whānau and our communities.”

RN Virginia Pugh, who works in orthopaedic outpatients in Wellington, said few were happy with the offer.
“Staffing is the key issue – we’re fearing for our jobs and patient safety,” she told Kaitiaki on the bus.

Wellington Hospital delegate Hilary Gardner told members at the meeting nurses were “at the end of our rope” and did not believe the offer was acceptable.
“When you get to the end of the rope, tie a knot and hold on. We are at the end of that rope – we’re asking you to tie a knot to hold onto with NZNO so we can go back to bargaining and try and improve this offer.”
Keneperu Hospital delegate Rose Reed asked the 500-plus NZNO members in the hall where all the new graduates were going. “Australia” was the shouted response.
“It’s not good enough” said Reed, talking about a lack of safety on wards, including for new graduates without adequate preceptorship.
“Ratios are not rocket science and if we can’t get the staff, we need someone to take action on the beds.”
Lack of support to attend stop-work
Wellington Hospital clinical nurse manager Ryan Teahan, who works in post-theatre recovery, said management had done little to support nurses wanting to attend the stopwork meeting.
“There are eight of us – I’m the only one here”.

They could have reduced the elective surgery list or brought in cover staff – but they were even more understaffed than usual, he said.

“They could have reduced elective surgeries and respected our legal right to attend a stopwork meeting.”
In Christchurch, three RNs from the opthalmology outpatient unit said there were 13 members who wanted to attend the meeting, but only three were able to.
Senior nurses’ pay
While most talked about dangerous understaffing, some raised the issue of senior nurses who had lost their own pay gap, as the RN scale had caught up to them through the interim pay equity adjustment.
Another bone of contention was Te Whatu Ora’s refusal to include a bargaining fee – meaning non-union members could benefit from union-driven pay increases without paying the usual “fee” they had always done.

Hutt Hospital delegate Nathan Clark said they wanted to put pressure on TWO for a better offer, as this one “falls well below inflation”.
Auckland delegate Ben Basevi said there was a “resoundingly unanimously high level of dissatisfaction” with Te Whatu Ora’s offer. “It’s actually pathetic”.
Along with the unsafe staffing levels, he said members were annoyed about the lack of pay relativity for senior nurses, who had now been overtaken by the RN scale, and the below-inflation pay offer.
Daniels said the turnout for a majority of meetings across the country had been greater than expected.
“I think nurses are absolutely sick and tired of being treated with total disrespect, with being left out in the cold, with being told by Te Whatu Ora they are just not going to talk about staff-patient ratios, to keep us safe at work, to not provide equity, and not provide relativity from senior nurses . . . ”











