“Essentially it pushes nurses out of the nursing role in the perioperative space — it means employers can employ a non-nursing health-care professional in that role,” chair of the NZNO perioperative nurses college (PNC) Cassandra Raj told Kaitiaki Nursing New Zealand. This was “very much a patient safety concern”.
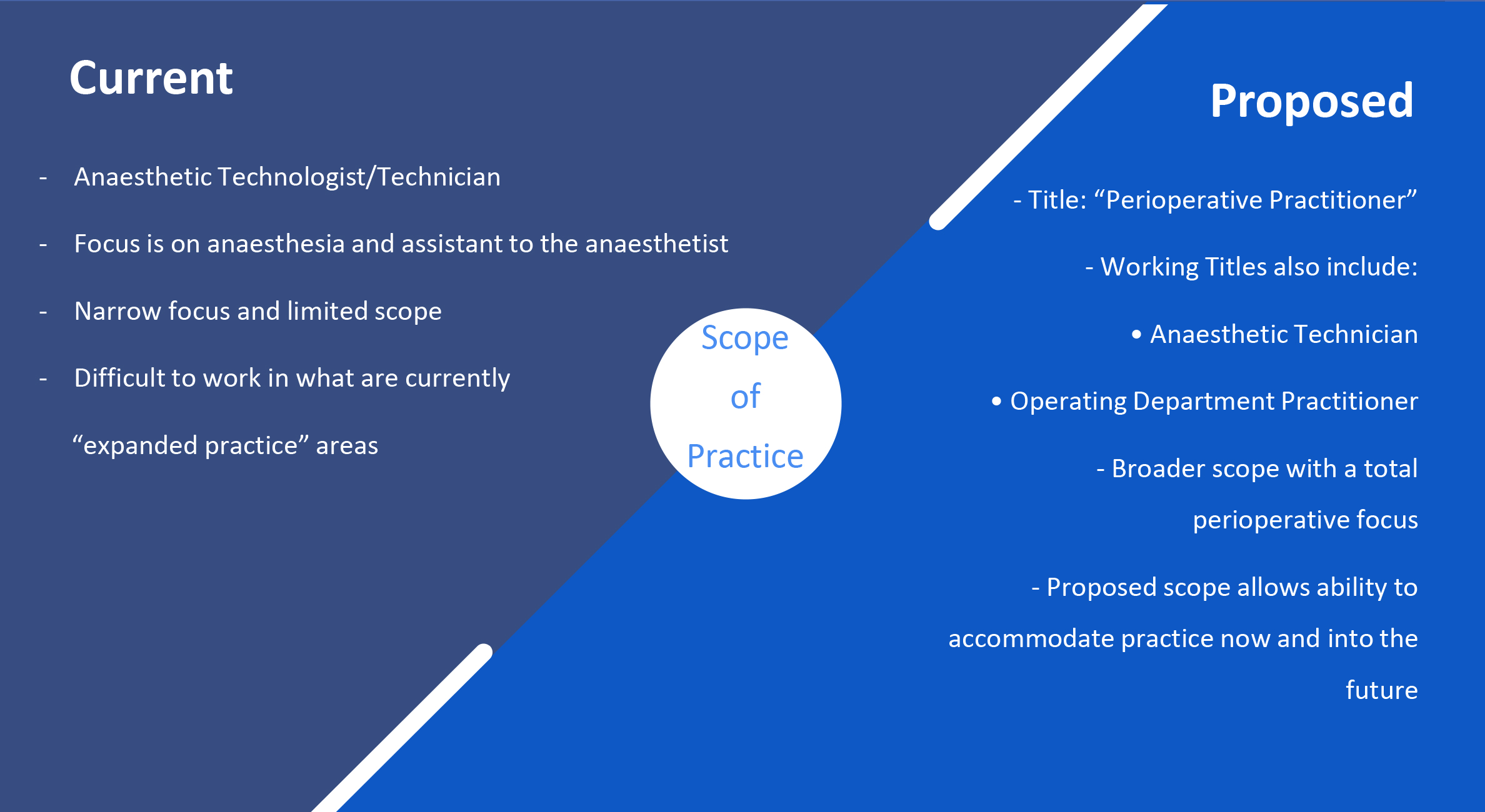
The AT profession’s regulator, the Medical Sciences Council, is proposing an expanded scope of practice to give them a “broader, more flexible” role. Instead of focusing only on anaesthesia and assisting the anaesthetist, they would also focus on “perioperative care”, including scrub and pre and post-operative care, the document states.
The proposed new title “reflects a more agile and broad scope of practice”, it said.
That meant the new practitioner role would be able to pick up specialty work in operating theatres usually carried out by nurses, Raj said. This might include circulating (coordinating surgical team and overseeing patient care before, during and after surgery), assessing the theatre, skill mix and patient complexity as well as having a “whole clinical and surgical consciousness of the operating theatre, all of the staff and their roles”.
The title was also easily confused with that of nurse practitioner — a role which took at least nine years to attain.

‘. . . you could have operating theatres run with no nurses in them. And that’s a concern for our patients’.
Until now, the AT role had been to assist the anaesthetist. While this was a vital part of the team, it was “very separate” to the nursing role, said Raj, a perioperative nurse for 22 years. But she feared the proposal would see them encroaching on the nursing role without the same level of knowledge, education and skills.
Raj said the proposal could ultimately lead to patients being cared for in theatre without a single nurse.
“If this was to come to full fruition, you could have operating theatres run with no nurses in them. And that’s a concern for our patients,” Raj told Kaitiaki Nursing New Zealand.
Education changes
At the same time, the two-year AT diploma at Auckland University of Technology (AUT) recently changed to a three-year health science degree, which will see 23 new graduates coming into the workforce next year.
They would be able to be employed as perioperative practitioners if the change in scope went ahead, as proposed, later this year.
Raj said it was “alarming” to think up to 23 new AT graduates might be looking after surgery patients next year without the appropriate skills.
“The three-year degree doesn’t show the skills and knowledge base that perioperative nurses have today to safely look after our patients.”
It was also unclear who would be responsible for clinical supervision of AT graduates when they started in the workplace, she said.
Overseas models
Pressure to expand the AT scope had been coming for many years from a group of health professionals originally from the United Kingdom (UK) called “operating department practitioners” — similar to the proposed perioperative practitioner — who wanted to introduce the model here, Raj said.
“This is also a historical battle that has been ongoing since the 1980s – it came up again in 2018 – and it’s really been wrapped up and pushed forward by strong vocal overseas practitioners.”
Raj warned perioperative practitioners could also step into other nursing specialties, with the flexibility to work in emergency, maternity, medical imaging, patient transport and radiology as well as post-anaesthetic care units (PACU). “They’re pitching themselves as such a flexible workforce.”

‘Contemporary’ workforce?
Medical Sciences Council chief executive Susan Calvert said the purpose of the review was to ensure ATs’ scope was “contemporary” and reflected a changing work environment and technology.
Asked about the impact on nurses, she said ATs were part of a team who worked collaboratively in a theatre environment. The council was seeking feedback before making any decision.
Calvert said the council’s role was to protect the health and safety of the public by ensuring ATs were fit and competent to practise their profession.
Consultation details
Consultation on the proposal is open till September 14. NZNO is preparing a submission and seeking member contributions. Please contact the PNC on [email protected].
The Medical Sciences Council is also holding two webinars on the proposal this week on Wednesday August 1 at noon and 7pm. Please email [email protected] to attend.