ICN has estimated the global shortage of nurses at around 5.9 million currently, with 89 per cent of the shortfall found in low and low-middle income countries — countries that can least afford to lose more nurses.
The shortage of nurses, factors that have contributed to the shortages and solutions that are being used, such as nurse/patient ratio legislation rather than unethical recruiting, dominated the presentations I attended.
The congress was held in Montreal, Canada, in the first week of July, hosted by the Canadian Nurses Association. Its theme was “Nurses together: a force for global health.”
Need for nurse/patient ratios
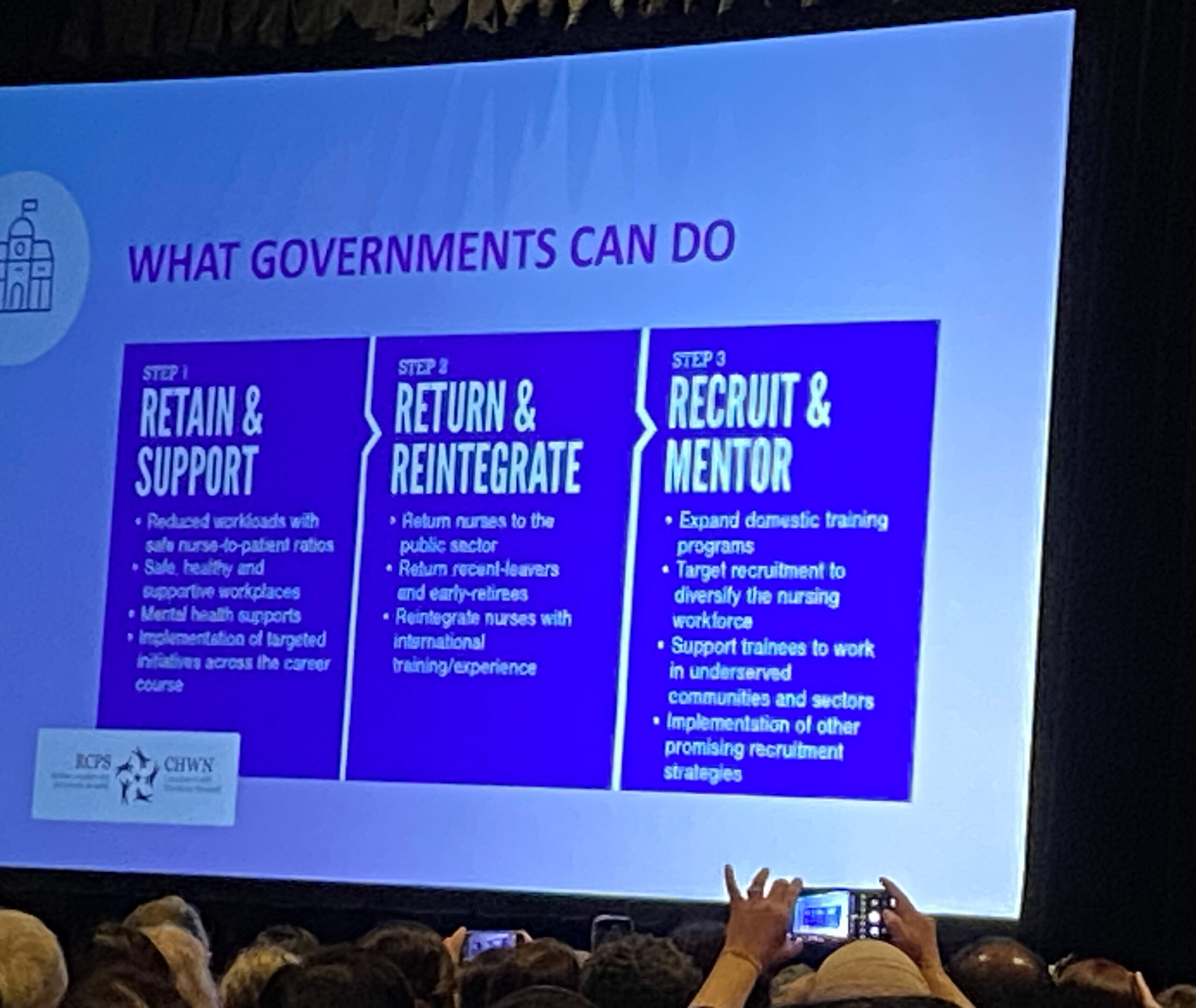
The need for legislated nurse/patient ratios is a priority for a growing number of nursing associations. ICN sees “patient safety and nurse staffing as two sides of the same coin”. It believes better ratios would improve recruitment and retention of nurses, reduce avoidable healthcare-associated patient harm, and support planning for the numbers of nurses and midwives required to support nations’ health needs.
On the issue of unethical nurse recruitment, ICN’s position is that “lower income countries should invest in the pay and conditions of their workforce and higher income countries should become more self-sufficient”.1 Despite calls for adherence to this position, this does not seem to be occurring.
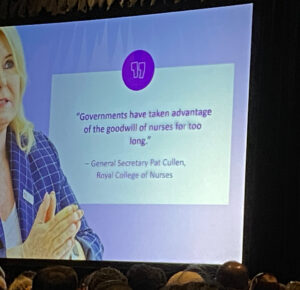
Unethical recruitment of nurses perpetuates the disparities and inequities between comparatively wealthy nations and those that struggle to meet the health needs of their people.
While it is important to uphold the individual rights of nurses to choose where to work, it was clear that recruiting IQNs as a stopgap measure to answer nursing shortages is not the answer to meet the needs of health care nationally or internationally.
Unethical recruitment of nurses perpetuates the disparities and inequities between comparatively wealthy nations and those that struggle to meet the health needs of their people.
So it was with some dismay that, on my return from the congress, I noted that the recently published Te Whatu Ora workforce plan has a stated heavy reliance on increasing IQN recruitment.

In New Zealand, there is a projected shortfall of more than 4000 nurses by 2032. The workforce plan relies on a reduction of student nurse attrition rates from 30 to 20 per cent and commits to “earn as you learn” — but is silent on what that might look like.
NZNO has, for a long time, clearly stated the strategies needed to meet the current and future health workforce needs of our nation. These include free fees and cultural and pastoral care for our nursing students, as well as retaining experienced and qualified nurse preceptors to support safe clinical placements. However these strategies were not evident in the workforce plan.
The NZNO student unit (based on a recent survey of nursing students) supports these strategies as appropriate responses to the huge financial, logistical, and family-focused challenges students grapple with, on a daily basis. Many countries presenting at the ICN congress spoke of similar challenges.
The need for legislated nurse/patient ratios is a priority for a growing number of nursing associations.
The ICN congress brought together national nurses associations (NNA) representing 28 million nurses worldwide. It focused on how the lessons learned through the COVID-19 pandemic could be used to
-
- protect nurses’ rights
- ensure decent working conditions and fair pay
- optimise nurses’ scope of practice
- drive nursing leadership and respect for the profession, and
- ensure nurses have a greater impact on health policies at all levels.
It was an opportunity for nurses to come together in solidarity, to learn from each other how we can turn the tide from illness to wellness in the context of safe health care.
It was the first time I had the opportunity to attend such an event, which presented both challenges and opportunities. The NZNO constitution requires the president to attend the ICN congress, so it was important for me to make the most of the time spent in Montreal on behalf of the organisation.
The conference had 152 presentations, plus poster presentations and master classes, running concurrently, in a variety of subjects, over five days from 7am to 6.30pm every day.
Considering our current New Zealand context, I was interested in exploring the experiences and activism of different nursing associations in protecting nurses’ rights, fair pay, and safe work conditions, now and in the future.
 Networking with nurses from around the world and from New Zealand (Nursing Council, Te Aka Whai Ora, nurse educators and clinical nurse specialists) resulted in a respectful interchange of ideas, research, leadership strategies and relationships.
Networking with nurses from around the world and from New Zealand (Nursing Council, Te Aka Whai Ora, nurse educators and clinical nurse specialists) resulted in a respectful interchange of ideas, research, leadership strategies and relationships.
The way forward for nursing involves us understanding what local, national and international policies will work best to tackle nursing shortages. This will help enable us to work together to eliminate health inequities and disparities, and show that nurses are a real force to be reckoned with, resulting in improved health and wellbeing for all.
Anne Daniels is the president of NZNO.
NZNO kaiwhakahaere Kerri Nuku’s view on the ICN congress can be found here: Holding hands across the globe — the power of indigenous nursing.
Reference
- International Council of Nurses. (2022, Aug 11). ICN calls for stronger codes for ethical recruitment of nurses and investment in nursing education (press release).



