Team work key, says nurse
A district nurse for two years, Charlotte Pudney said after noticing the inflamed eye, she ended up sending ophthalmologist James Lewis a photo via cellphone. “Because she’s housebound and it was the weekend, I couldn’t get her into the GP or to ED [emergency department].”
“He organised her to come in — which is really hard to do with patients in the community, get them help when they need it, especially at the weekend.”
The patient ended up at ED that afternoon and was home for dinner. “She was so happy — because that one eye was her good eye and she’s housebound, so her life is reading.”
Pudney knew the patient — who had daily district nurse visits — well and said warning bells kicked in when she saw her eye.
“They call it the nurse’s sixth sense.”
During a routine home visit to change a leg dressing, Wellington community nurse Charlotte Pudney noticed her elderly patient seemed unusually uncomfortable, frequently rubbing her eye, which appeared red and inflamed.
Trusting her intuition — a skill honed through years of close patient interactions — the nurse chose to investigate further. Her experience in recognising subtle signs that something was “off” — a characteristic trait among seasoned health-care professionals — prompted her to act on a hunch, despite the primary focus of her visit being wound care.1, 2
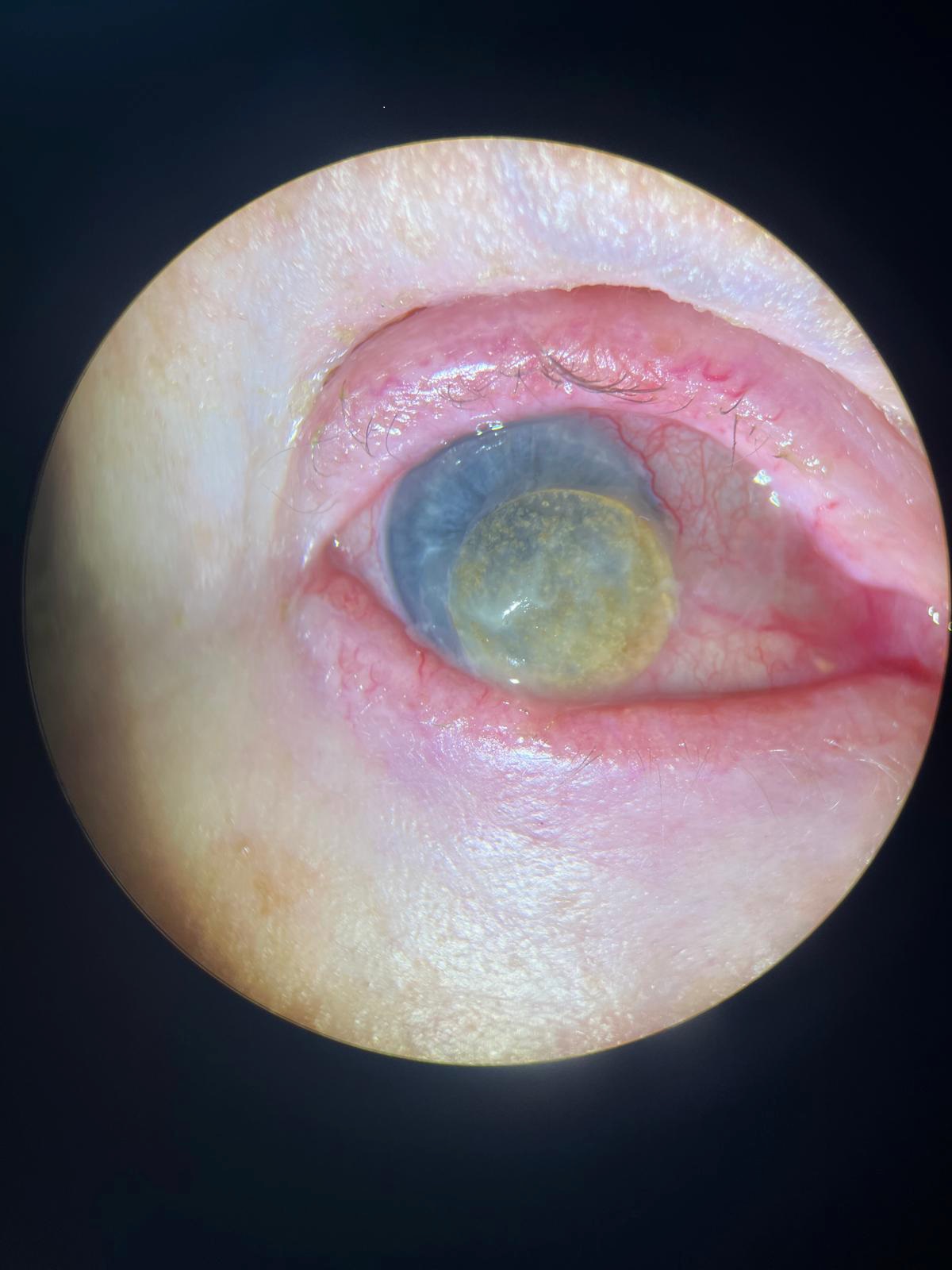
‘ . . . examination revealed a hard contact lens, concealed for approximately five years’.
The nurse’s concern led to a referral to the emergency department, where examination revealed a hard contact lens, concealed for approximately five years, had shifted and was causing irritation.
This discovery enabled prompt treatment with an antibiotic ointment, leading to rapid recovery. Further assessments revealed untreated vision issues, including cataracts, macular degeneration, and uncorrected shortsightedness.
Research shows that experienced nurses and midwives frequently use “embodied intuition” to detect subtle changes, relying on physical cues and a sense of knowing when something isn’t right — qualities shown to improve patient outcomes.3, 4

This case exemplifies the importance of “embodied intuition” and “clinical intuition” in nursing and midwifery.
‘Research shows that experienced nurses and midwives frequently use embodied intuition to detect subtle changes, relying on physical cues and a sense of knowing when something isn’t right.’
In fast-paced or complex care environments, these health-care professionals often respond to subtle, sometimes unspoken, patient cues, recognising inconsistencies between reported and observed symptoms that may indicate a deeper issue.
Experienced nurses and midwives have been shown to rely on intuition in challenging scenarios, which, as research suggests, is a vital element in patient safety and effective clinical decision-making.5, 6

Nurses and midwives are uniquely positioned to leverage this intuitive skill due to their frequent, close interactions with patients. The ongoing relationship they develop often allows them to detect gradual changes in health that might otherwise go unnoticed.
This case also reminds midwives, who support mothers and newborns through critical health stages, of the value of trusting these instincts. Just as nurses use intuition to detect shifts in an elderly patient’s wellbeing, midwives can apply their insights to identify early signs of complications, promoting timely interventions.2
Nurses and midwives have years of education and experience in patient care, and should trust their instincts. Even small observations can lead to significant health-care interventions, reinforcing the importance of intuition in providing the highest standard of patient care.
- James Lewis is a Wellington ophthalmology registrar
References
- Benner, P. (1984). From novice to expert: Excellence and power in clinical nursing practice. Addison-Wesley.
- Payne, L. K. (2015). Toward a middle-range theory of intuitive decision-making in nursing. Nursing Science Quarterly, 28(3), 223-229.
- Muoni, T. (2012). Decision-making, intuition, and the midwife: Understanding heuristics. British Journal of Midwifery, 20(1), 52-56.
- Jefford, E., Fahy, K., & Sundin, D. (2011). Decision-making theories and their usefulness to midwifery practice and education. International Journal of Nursing Practice, 17(3), 246-253.
- Evans, J. S. B. T., & Stanovich, K. E. (2013). Dual-process theories of higher cognition: Advancing the debate. Perspectives on Psychological Science, 8(3), 223-241.
- Ménage, D. (2016a). A model for evidence-based decision-making in midwifery care: Part 1. British Journal of Midwifery, 24(1), 44-49.