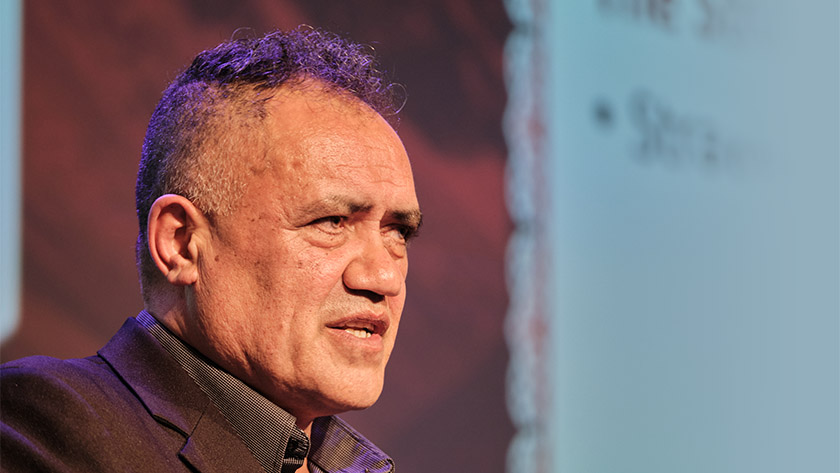
Rawiri Taonui, speaking to the Indigenous Nurses Aotearoa Conference 2021, spoke with a kind of calm resignation about the future of the pandemic in Aotearoa.
Less than a week later, he was proven correct.
In a wide-ranging discussion of racism and how it played out historically in causes and responses to outbreaks, Taonui said there would likely be community transmission of the virus before the year’s end.
A researcher and semi-retired professor of Māori and indigenous studies, Taonui said he wasn’t a medical doctor. “But I do have the ability to diagnose and recommend treatment for racism.”
He said racism itself was a virus.
‘When the racist looks at you, and us: all the bad things they think about humanity, they see in us… but when they go home and look in the mirror they see all the good things in humanity.’

Over time that created a kind of “historical amnaesia”, with society unable to see the wrongs perpetrated in the past.
“Fundamentally they cannot get over the fact that they are ‘good’, ‘helpful’, ‘superior, ‘advanced’.”
There were multiple phases of epidemic and pandemic events for Māori in Aotearoa, he said – beginning with first contact with Europeans who spread new diseases among Māori, who had no immunity to them.
This first episode was in 1769, when James Cook’s crew spread sexually transmitted diseases such as gonorrhoea and syphilis among Māori in Golden Bay.
This was the first of a series of about 20 pandemic and epidemic events affecting Māori before the signing of Te Tiriti in 1840.
He said about 70 per cent of the Māori population died from disease and muskets in the 70 years since the Cook contact.
Diseases continued to ravage the Māori population through to the 20th century.
Racism had also affected the rollout of vaccines. Taonui pointed to a 1913 smallpox epidemic, started by a visiting American missionary.
The missionary spread the disease at a hui with Māori. More than 700,000 vaccines were made by the government, but distributed to mainly-European towns.
“Whatever was left over was distributed amongst Māori communities.” He said at the time, no Māori were even allowed to administer the vaccine.
The influenza epidemic after World War I saw health services favour Pākehā, with Māori often left to look after themselves, he said.
This unequal treatment for Māori continued through the century to the modern day.
Taonui said when COVID-19 arrived in Aotearoa, the Government formed a response group with no Māori members.
“The Ministry of Health manage a $22 billion a year budget, I think there’s about 300 people that work in headquarters in Wellington.”
When the pandemic arrived, they employed “zero” Māori doctors in that office, he said.
There were disparities for accessing COVID-19 testing for Māori and Pasifika communities in the early stages of the pandemic he said.
“So basically what happened is Māori health providers just decided to break the rules, and test the communities.”
These providers received criticism from media, but simply carried on.
“Within two weeks, all DHBs took the same approach: Go out to Māori communities and just test everybody you can lay your hands on.”
The latest problem was the vaccination rate for Māori – running at about half the rate of the general population.
“The first thing people ask me is ‘why is there such vaccine hesitancy?’ I say, ‘Well I don’t think there is that much’.”
There was a one-size-fits-all strategy, rather than setting up priority communities based on social, demographic and geographic profiles.
He said Delta was dangerous and Māori needed to get as many people vaccinated as possible.
“If Delta comes to New Zealand, I think it probably will, we’ll probably have an outbreak before the end of the year, we’ll need as much protection as we can.”
Less than a week later, Prime Minister Jacinda Ardern announced the country would go into alert level 4.
Little over a week after that, the case numbers rose to more than 500 people, in Auckland and Wellington.
While the Pfizer vaccine was one of the best in the world, it was made to fight the earlier strains of the virus, Taonui said.
“Even if you’ve been immunised, you can still become infected. The chances of surviving are much better, your chances of becoming hospitalised or dying are much smaller. But you can spread it to other people.”
Borders should not be opened too much before at least 80 per cent of the population were immunised.
The health community needed to do as much as possible to help Māori get vaccinated, he said.