Trauma nurses work in all acute hospitals across New Zealand. On a day-to-day basis, the trauma nurse is a key part of the trauma patient’s journey, providing care for the approximately 2400 people who suffer major trauma each year on our roads, or from falls, assaults and other causes. Major trauma is associated with around a 10 per cent mortality rate and for those that survive, many have serious disability requiring long-term rehabilitation. There is a disproportionate burden of trauma on Māori, while the financial and societal cost is significant for everyone.
The National Trauma Network was established as a contemporary system of care in New Zealand to improve outcomes for those who with serious injuries. Historically, we have seen unwarranted variations in care, and adverse outcomes such as high mortality rates. Trauma nurses, along with their trauma colleagues, are credited with the improving performance measures we are now seeing. The mortality rate is reducing, and most processes of care are improving. We have set up a population-based trauma registry, a formal system of care, and approximately 30 trauma nurses with dedicated time in each acute hospital.
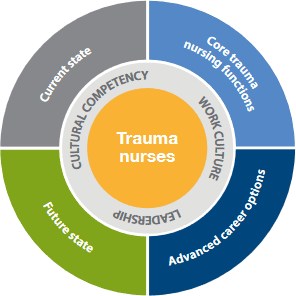
But what is a trauma nurse? Until recently, we had no common view, so a working group of trauma nurses, representing small and large hospitals, set out to define the core components of the role and articulate the ambitious vision for the workforce over the next five years.
Four core functions of the trauma nurse role were identified:
- Data collection on all patients who meet the threshold for inclusion to the major trauma registry. This registry is the foundation for data-driven quality improvements in trauma and the unique injury coding allows us to benchmark nationally and internationally.
- Case management: Trauma patients often require complex, coordinated care through their hospital stay. Case management is an excellent approach to ensuring they receive optimal care of their physical, social, cultural and mental health issues.
- Quality improvement: An effective system is one where improvement is done at all levels of service. This year, 20 nurses and allied health staff will begin quality improvement facilitator training to strengthen our national focus on critical haemorrhage, serious traumatic brain injury and rehabilitation.
- Education of patients, their whānau, other staff, and the community. Serious injury can have a profound effect on the individual and their community, and education plays an important role in supporting optimal recovery.
Our goal is for all trauma nurses to have these core functions included in their role. How this is done will differ between small and large hospitals, but we understand that implanting this approach will result in better outcomes for our patients.
Hospital executives who make investment decisions and allocate hospital resources would be interested in the tangible benefits of the trauma nurse role. There is good evidence linking trauma nurses and reduced bed days, reduced acute unplanned readmission, reduced complication rates, improved referral and patient management pathways, and improved patient satisfaction.
Nationally, there have been significant improvements in the capacity and capability of the trauma nursing workforce. Many trauma nurses have completed or are undertaking a clinical masters, with potential to become nurse practitioners.
However, there are a small number of hospitals where the role is seriously under-resourced for the caseload. The health sector tends to drive high performers the hardest, and this is true in these hospitals. A trauma system is just that: a system; and if one part is stretched beyond reasonable capacity, it has an impact across the whole system.
Notwithstanding these challenges, the commitment of trauma nurses is demonstrated by a culture of professionalism and continuing education to improve patient care. This means we are in a much better position now to provide optimal care of the injured person.
We are ambitious to increase the trauma nursing workforce, and with support from ACC, nurses receive financial assistance to train, attend conferences, and continue professional development. We would like to see at least one specialist trauma nurse practitioner in each region’s tertiary centres over the next few years. We would like to see more Māori nurses identify trauma nursing as a specialty.
It’s an exciting time to be a trauma nurse in New Zealand, and to be part of a nationwide effort to develop a world-leading trauma system.
More detail on the professional development framework for trauma nursing can be found in the Trauma nursing professional development framework (PDF, 1.21 MB) while the Major Trauma website has more information on the National Trauma Network.
Report by Siobhan Isles, RN, MSc, national programme manager, National Trauma Network




