In her presentation, Whai Oritetanga – In pursuit of equity, Haddon, who is the quality and service improvement manager, Māori Pae Ora Māori Health Directorate at MidCentral District Health Board, posed many questions about how nurses cared and advocated for whānau and how they applied te Tiriti o Waitangi in their practice.
“As nurses, how can we create new ways collectively to ensure whānau can access care, free from judgement and have the knowledge to advocate for themselves? How, as nurses, can we enable culturally relevant support? Do we put ourselves in someone else’s shoes? Do we understand their opinions and point of view? Often, as nurses, we focus through an individualistic lens, whereas we should place the entire whānau at the centre of everything we do.”
‘If you change the way you look at things, things you look at will change’
Haddon (Ngāpuhi) defined equality as treating everyone the same; equity as providing the resources people needed to get ahead and liberation as removing all barriers and including considerations such as whose whenua you were on and incorporating iwi.
Māori health equity involved deliberate actions to make sure “we are doing our best for whānau”, including integrating bicultural practices in everything we do.
Haddon repeated a number of statements Māori nurses heard every day:
“I treat all people the same, regardless of ethnicity.” “They have too many people visiting them.” “Māori patients are too complex.” “They live outside this region.” “I’m not from New Zealand and I haven’t heard of the treaty.” “Working with whānau is not as important as working with the patient.”
And Māori patients often told Māori nurses: “I’m not talking to them because I feel they judge me and my whānau.” “I just tell them what they want to hear.”
Hearing those sorts of statements every day was sad. She urged nurses to shift to a wellness focus, to engage in whānau-centred practices and to consider how, collectively, they could advance Māori health.
“Do you connect across services or stay within your own speciality?” she asked.
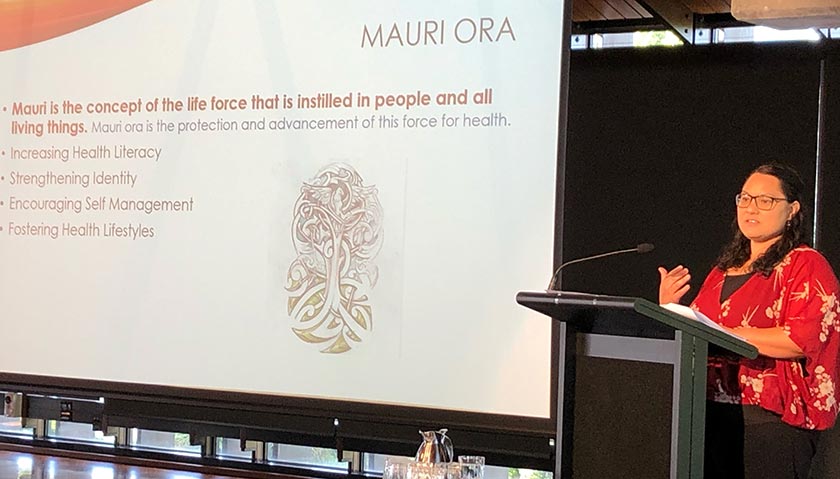
Mauri ora
Nurses should use the concept of mauri ora – life force or an essence – to help Māori they cared for to increase their know- ledge and their power and to restore their dignity. The concept of waiora referred to the significance of the environment on wellbeing. The environment included good housing, clean water and air and healthy kai.
Partnering with whānau, using whānaungatanga when introducing yourself, asking whānau what mattered to them and what resources they needed, working with iwi providers and kaupapa Māori services and referring whānau to them, including whānau in multidisciplinary team meetings and using Māori models of health were some ways nurses could “broker and create therapeutic relationships with whānau”.
How do nurses advocate?
Nurses should also consider how they advocated for those in their care and Haddon posed some questions to consider. From whose perspective? Who do we involve? What does it look like? What does successful advocacy look like for whānau?
She challenged nurses to “think differently. If you change the way your look at things, things you look at will change”, she concluded.
In her mihi, she referred to those who had died of the corona virus and to the 185 people who had died in the February 2011 earthquake in Christchurch – “aroha and respect to all involved”, she said.
Haddon also provided some historical context to her presentation, stating that Māori health had been undervalued since the early 1800s. The Tohunga Suppression Act, 1907, had grown out of Western ideology and had forced rongoā practices underground. “That Act denied the ability for us to have culturally responsive practices.”
Nursing education had been modelled on the Florence Nightingale schools. “The way schools were run dismissed how we practised and indigenous knowledge was removed from the curriculum.”
This professional forum coverage replaces college and section news for March.