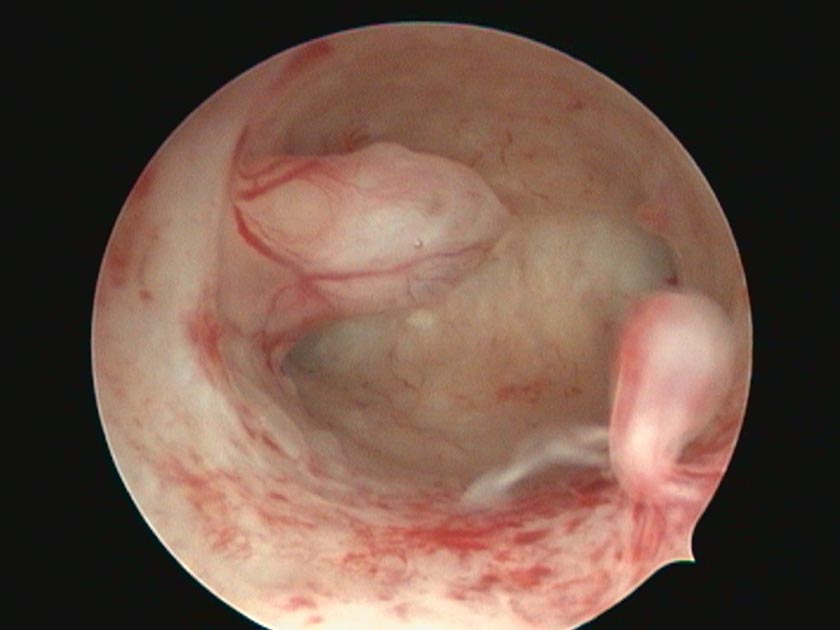
Moore is the only nurse in New Zealand training as a hysteroscopist, a role which involves examining uteri, often for cancerous or pre-cancerous conditions.
She began training in August 2020 on a pilot programme at Waikato District Health Board (DHB), developed by head of gynaecology Dr Tavaziva Mudzamiri. Currently on maternity leave, she hopes to finish in 2022.
With a “forever increasing” waiting list for women requiring hysteroscopies to diagnose pre-malignant or malignant conditions, the gynaecology team had struggled to keep up, she said.
Until now, hysteroscopies have primarily been the domain of gynaecologists in New Zealand, unlike the United Kingdom (UK) where nurses had been performing the role for 20 years.
Having worked alongside many nurse hysteroscopists in the UK, Moore said Mudzamiri was keen to introduce the concept to Waikato DHB to help speed up cancer diagnoses and treatment and reduce waiting times for women – with the ultimate aim of improving health outcomes.
Moore says having a permanent nurse hysteroscopist at women’s health outpatients would provide continuity of care and a “holistic” approach where broader needs can be met.
“This is an extremely frightening and vulnerable time for women – having a female hysteroscopist is a significant benefit”.
Already working as the DHB’s only nurse colposcopist, examining the cervix, Moore had been able to offer women regular weekly clinics. A permanent nurse hysteroscopist would have the same benefit of consistency and reassurance.
Moore said as a women’s health NP and nurse colposcopist she was “instantly attracted” to the idea of training for this position, “leading the way for other nurses within New Zealand”.
The training standards are adapted from the British Society for Gynaecological Endoscopy and the programme – run over 12-18 months – combines theory and practical elements. Her clinical mentor is obstetrics and gynaecology consultant Sean McConnell, who had given many hours of training to both inpatient and outpatient hysteroscopy, she said.
The pilot programme was intended to test how to successfully complete hysteroscopy training for nurses in New Zealand.
Moore is also helping develop NZNO Women’s Health College (WHC) national hysteroscopy training standards. They will form the basis for a polytech-based hysteroscopy training programme for nurses hoped to be launched in New Zealand in 2022, Moore said.
Endrometrial cancer, which affects the uterus lining, is one of the fastest-growing cancers in New Zealand, but about 80 per cent of cases can be treated if detected early.
Training nurses to provide this care would make it more available and equitable and save lives, Christchurch NP and colposcopist Jill Lamb has said.
Endometrial cancer rates were disproportionately high in Māori and Pacific populations, with wāhine Māori mortality rates almost twice that of non-Māori.
Lamb said she hoped to see nurse-led hysteroscopy services available throughout Aotearoa.