
Our health system is struggling in the face of growing demand. While there are obvious problems that need to be fixed immediately, we need a change in how we fund it in order to have a truly comprehensive public health system that is free at the point of use.
Right now, emergency departments across the country are bursting at the seams with many more people needing emergency care than there are nurses and doctors available to provide it.
Our cancer services are under enormous pressure (particularly in the South Island) and the shortage of doctors, nurses, midwives and other types of health workers right across the system means many of us can’t access the care we need. This lack of access particularly affects Māori and Pacific peoples as well as other disadvantaged groups.
An ageing and growing population, closure of aged care facilities, despite 13,000 beds being needed by 2030, is adding to the pressures on primary and tertiary care providers, where resources have not met demand for a long time.
These challenges come on top of longstanding issues we have had with our public health system. Some examples are:
- Ever since its beginnings in the 1930s, the dental health system has never been fully publicly funded. This has caused unnecessary suffering every day as people can’t afford to see the dentist and dental problems go untreated.1
- Our Pharmac pharmaceutical purchasing system is generally recognised as a success but is still not funded enough to meet demand.2
- Our health system has struggled with access and equity issues for years.3
- Hospital buildings have long been in need of a make-over — in 2020 the Government released a stocktake of hospital infrastructure which put the fix-it bill at $14 billion over the next decade.4

We have seen significant increases in health funding over recent years, following a decade in which funding failed to keep up with population growth and increasing health costs. Budget 2022 delivered record levels of investment, but these were described by the Minister of Finance as a one-off, designed to help clear the decks for the new health structures.
The reality is that even with the increases over recent years, our spending per capita on health is less than many comparable countries.5
While our ranking in the OECD has improved from 19th in 2020 to 14th in 2022, if we were to have a health system that was truly comprehensive and free at the point of use (such as the National Health Service in the UK) it has been estimated that we would need an extra $3 billion a year in funding,6 year on year.
We need to significantly grow tax revenue to fund the health system we need.
This would help address the issues identified above, including helping us pay the wages we need to compete internationally for nurses and other health workers. However, we do not collect enough revenue through taxation to enable this to happen and we need to significantly grow tax revenue to fund the health system we need. In short, we need to talk about tax.
Challenging beliefs about tax
Part of that conversation must be to challenge the widespread belief that Aotearoa New Zealand has high tax rates. The revenue collected in 2021/22 represented a higher proportion of GDP than has been the case for most of our recent history and probably reflects the impact of COVID-19.
However, it is lower than the OECD average and significantly lower than many of the countries we like to compare ourselves with, such us Germany and the Nordic countries. Tax revenue as a percentage of GDP in 2021/22 was 33.78 per cent in this country, compared with 39.51 per cent for Germany and 42.58 per cent for Sweden.

It is no coincidence that these countries also spend more per capita on health than we do. If we taxed at the level of the Germans, we would have somewhere between $20-$30 billion more to spend on the things we urgently need, including health.
With polls telling us that most people would like a tax cut, where would this money come from? The short answer is that it needs to come from those who can most afford it. Our current tax system asks too much from those who can least afford it, while not enough from those who can.
Too reliant on GST and income tax
We rely too heavily on GST and income tax. In 2021/22, individual income tax accounted for 51 per cent of tax revenue and GST for 25 per cent — higher than the OECD average. GST is a regressive tax – it is levied on virtually everything we buy and therefore impacts more heavily on the least well off.
Our income tax system is also unusual in that it doesn’t have a tax-free band at the bottom, so once again it is the least well off who are affected.
Our tax system helps drive inequality.
The other thing to note is that these taxes are almost impossible to avoid – everyone who is employed has to pay income tax and GST applies to just about all goods and services (although that might change, depending on the outcome of the election).
At the other end of the economic spectrum, income from capital gains is barely taxed in this country, which makes us an outlier internationally. There is the “bright line” test on houses other than the family home, which taxes those properties if they are sold within 10 years of being purchased, but there is no tax on income from other capital gains such as the sale of shares.
There are also no wealth tax and no inheritance tax (which is unusual within the OECD where 24 countries levy such a tax).
Research shows tax inequity
The resulting inequity was demonstrated by research conducted by Inland Revenue and released in March this year,7 which found that the effective tax rate for the wealthiest 311 families in Aotearoa New Zealand (who generally have a net worth of more than $50 million) was 9.4 per cent, compared to 22 per cent for a middle-wealth New Zealander.
So our tax system not only does not gather enough revenue, its structural inequities contribute negatively to the social determinants of health. It helps drive inequality and impacts on the income of the least well off and their ability to house and feed their families.
So it is time to talk about tax and to look at serious reform if we are to get the public health system we need, and to enable us to compete internationally for the nursing workforce we need.
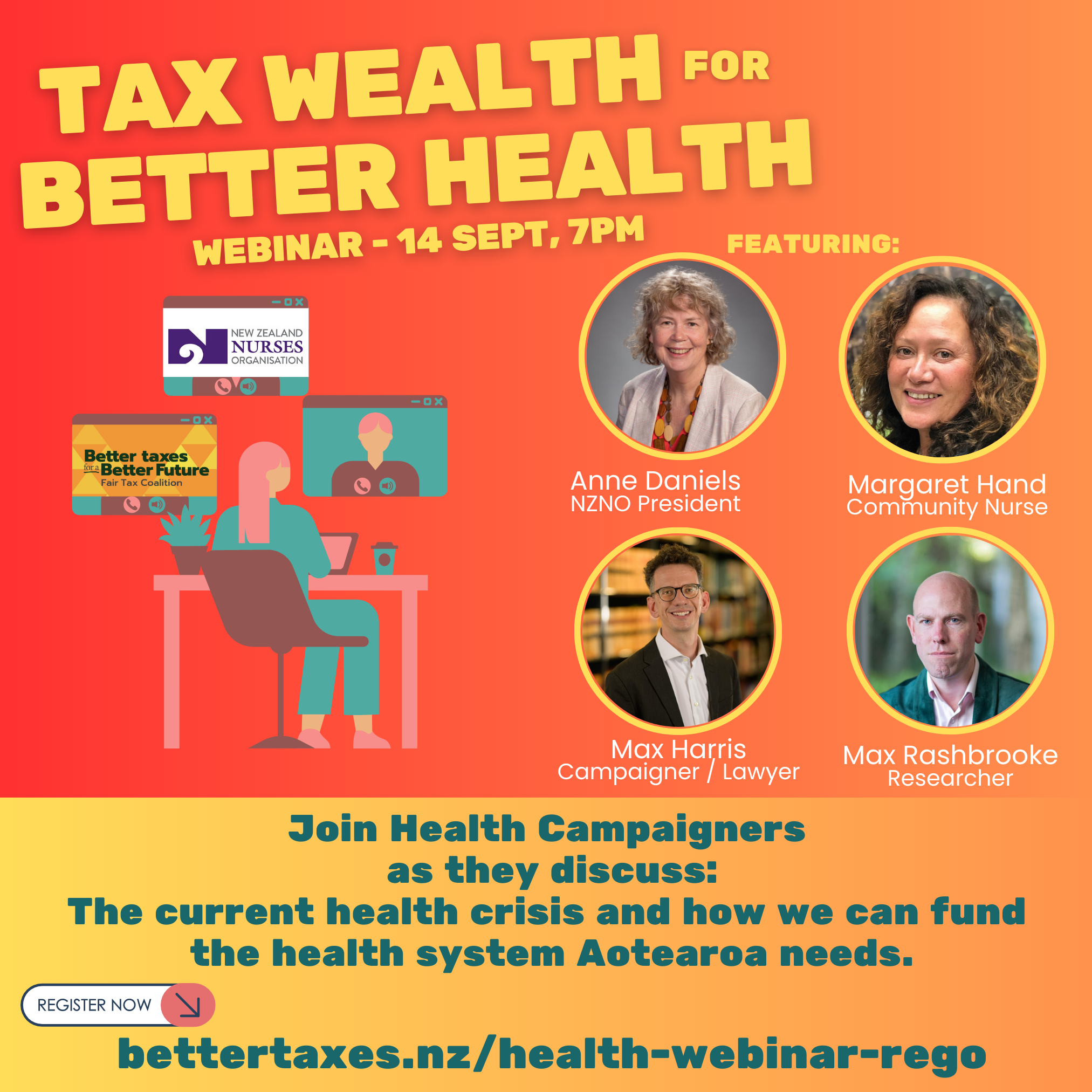
Glenn Barclay is the chair of the Better Taxes for a Better Future campaign.
Anne Daniels is the president of Tōpūtanga Tapuhi Kaitiaki o Aotearoa — NZNO.
References
- Glenny, H. (2022, April). The shocking state of dental care. North & South.
- Neilson, M. (2021, April 20). Pharmac drug-buying wish list needs extra $400m; calls for review to include funding. NZ Herald.
- Health and Disability System Review. (2019). Health and Disability System Review — Interim Report. Hauora Manaaki ki Aotearoa Whānui – Pūrongo mō Tēnei Wā.
- Pennington, P. (2020, June 10). The state of our hospital facilities: New stocktake paints dire picture. RNZ News.
- Organisation for Economic Co-operation and Development (OECD). (2023). Health spending (indicator).
- Rashbrooke, M. (2022). Lightening the load — the case for a fully free public healthcare system (p. 16). ASMS.
- Inland Revenue. (2023). Tax and the economic income of the wealthy.





