Some of what we did would be almost laughable today. For example, we put on a short-sleeved cloth gown when entering the room of a patient in isolation. When we left the room, we carefully removed the gown and placed it on hooks on a metal stand, ready for the next person to put on and remove in the same way. We did not use gloves for much and when we did, they were plastic and far too big for our hands. We washed our hands with soap and water, and they often became raw and sore. How times have changed. Standard precautions, the use of personal protective equipment (PPE) and the application of the five moments of hand hygiene have completely changed the way patients are cared for.
‘Pandemic clock ticking’
Infection control nursing has evolved into a specialist nursing role with the emphasis now on prevention rather than control. This has become even more important as the upsurge in multi-resistant organisms and communicable diseases challenge us daily. I remember a speaker at an American infection prevention and control (IPC) conference I attended many years ago saying the pandemic clock was ticking, but we just didn’t know what time it was. Well we do now! SARS-CoV-2 (aka COVID-19) has changed everything. We should have been prepared for it, but when reality hit, we found we were not.
Questions and more questions
As an IPC nurse for more than 20 years, things I thought I knew were turned on their head, as the overwhelming tide of new information, some of it contradictory, flooded in. Was COVID-19 droplet borne or was it airborne? Should we wear an N95 mask or a surgical mask, or both? Should we be using powered air respirators? Should we use face shields or should we use goggles? Should the patients be nursed in a room with negative pressure or could they be nursed in a normal room? Then there were fears about whether there was enough PPE; whether we could we pass it on to our families at home; and whether you could refuse to look after a Covid-19 positive patient. And there are so many more questions and still no clear answers to many of these questions.
What is important, however, is where information is sourced from and that the advice given is consistent. For my workplace, the Ministry of Health (MOH) became the voice of “truth” that cut through the many different opinions on how we should be doing things. While initially confusing for some, using the MOH guidance documents helped provide clarity and certainty for staff that what we were doing was current best practice.
The impacts of COVID-19 were many, particularly when hospitals were closed to visitors, and infection prevention rules meant families could not be with their loved ones even when they were dying. This particularly affected the Māori concept of whānaungatanga, in which relationships and family connections are so important. The tikanga around death and dying had to change, as families had to use telephones or online meetings instead of being there and health-care workers performed karakia instead of the usual spiritual advisers.
As an IPC nurse for more than 20 years, things I thought I knew were turned on their head, as the overwhelming tide of new information, some of it contradictory, flooded in.
Not all the effects of Covid-19 were negative. The number of influenza cases dropped to almost none. This proved that, along with vaccination programmes, basic infection prevention measures, such as frequent hand hygiene, cough and sneeze etiquette, social distancing and not coming to work when sick, worked. Mask use has become part of the way things are done and I have had many staff tell me they now realise they should have been doing some of what they are doing now, all the time.
A continued emphasis on good IPC practice will help prevent many other diseases from spreading as IPC is not something we do when we are facing an imminent threat – it is part of what we should be doing all the time. In time, Covid-19 will go away but we cannot afford to be complacent – there will be something else waiting to come along.
Finally, I want to say thank-you to all the many different health-care workers who have been, and still are, working so hard to screen for, and manage the care of suspected or known COVID-19 patients. At this time, it is those working in the managed isolation and quarantine facilities and doing the swabbing in the community that are at the forefront of efforts to keep COVID-19 out. But together, we have all made a difference.
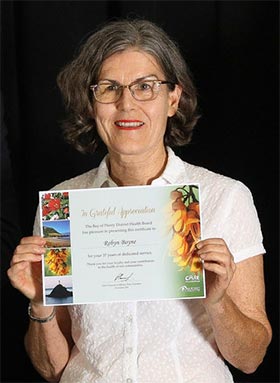
Robyn Boyne, RN, BN,PGDip (HlthSci) is a clinical nurse specialist in infection prevention and control at Bay of Plenty District Health Board.



